Front-desk teams drowning in phone calls, scheduling headaches, and a never-ending pile of paperwork. Doctors are running behind schedule again. Burnt-out nurses are multitasking nonstop: checking vitals, prepping rooms, logging data.
And patients? They’re waiting. Waiting for someone to answer, to explain, to just be available.
It adds up. No-shows become routine. Follow-ups fall through. Engagement drops. And at the bottom line? Lost revenue.
That’s usually when leadership starts looking for answers — not more staff, but smarter systems. Which is probably why you’re here, weighing the value of conversational AI in healthcare.
Spoiler: you’re on the right track.
In real-world trials with conversational AI, the system replaced workflows of 100+ full-time employees and delivered 4× faster processing for tasks like prior authorization and insurance communications.
But no technology is a silver bullet.
Where does conversational AI thrive, and where does it stumble? And if you're thinking about building a custom healthcare conversational AI, what should you know before taking the leap?
I’m Oleh Komenchuk, ML Lead at Uptech, a product development studio that works across several industries, with healthcare being one of our core domains.
In this article, I’ll break down what conversational AI for healthcare really looks like and how to make sure it works for your business, not the other way around.
Let’s get into it.
Benefits of Conversational AI in Healthcare
Once you start looking at conversational AI seriously, the real question becomes where it can deliver the greatest benefits. Here are the areas where it tends to have the biggest impact in healthcare.
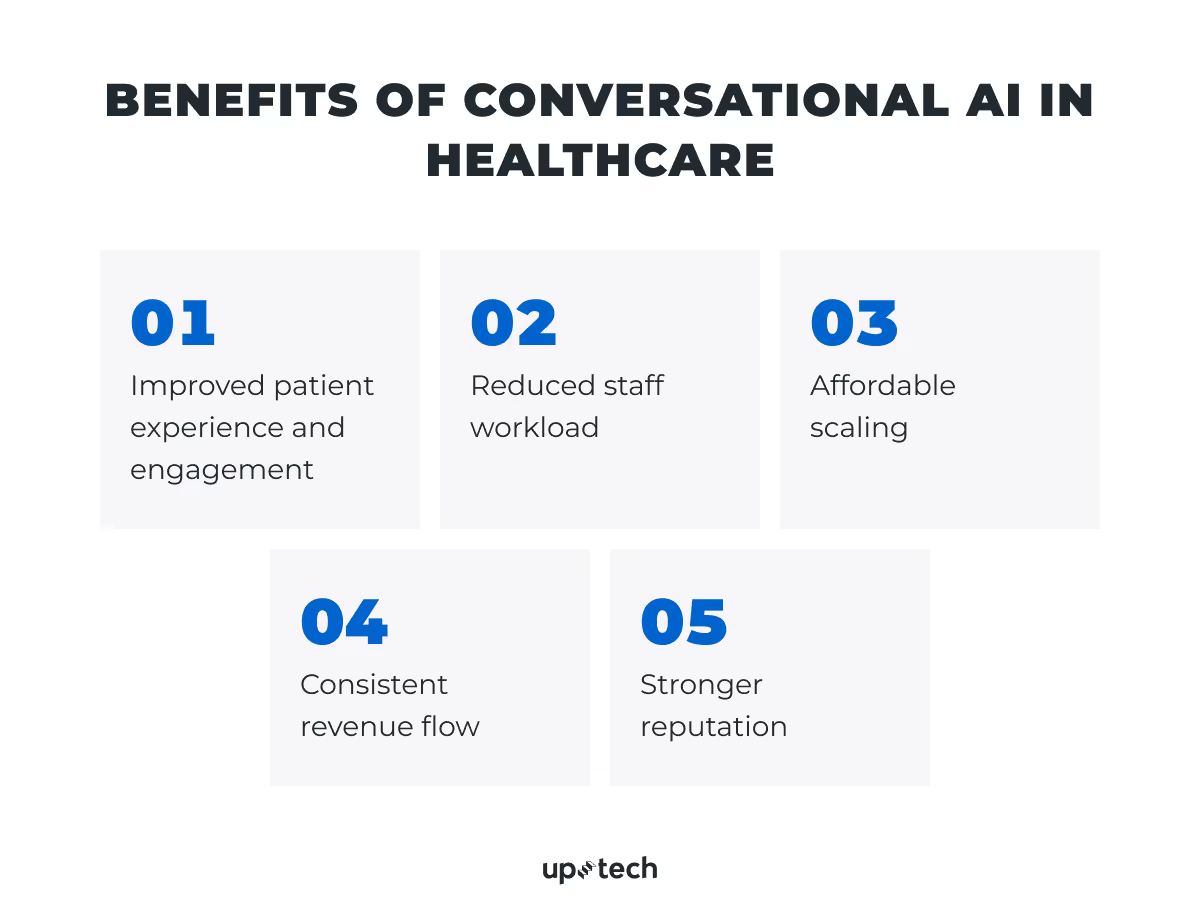
Improved patient experience and engagement
Faster, clearer communication keeps patients engaged and confident in their care. Conversational AI provides instant answers any time of day, explains information in plain language, and manages routine requests without staff delays. Patients spend less time waiting and more time moving forward in their care, leading to higher satisfaction and stronger retention.
Reduced staff workload
By taking over repetitive admin work, conversational AI frees clinicians and support teams to focus on patient care. Less time spent on clerical tasks means lower stress, reduced burnout, and fewer costly errors, creating a more sustainable work environment.
Affordable scaling
AI-powered automation allows healthcare organizations to handle more patients and locations without proportional increases in staff or expenses. As demand grows, these systems absorb the additional workload, maintaining service quality while keeping operational costs in check.
Consistent revenue flow
Automated reminders, rescheduling prompts, and follow-ups reduce no-shows, keep patients on track with treatments, and ensure billing isn’t delayed by missed steps. This steady patient flow protects revenue and maximizes the use of provider time.
Stronger reputation
Reputation in healthcare goes beyond clinical outcomes. It's shaped by how patients are treated at every step — from booking to follow-up.
Conversational AI gives you a way to deliver consistent, timely, and empathetic communication at scale — reinforcing patient trust and strengthening your brand with every interaction.
Use Cases of Conversational AI in Healthcare
If you’re here, chances are you already know what conversational AI is. Maybe you’ve sat through a few demos, maybe you’ve skimmed a vendor brochure or two. The concept makes sense.
But the real question still stands:
Is it actually worth implementing — in your environment, with your systems, your constraints, and your priorities?
Let’s skip the theory and get practical.
Below are the core operational areas where teams apply conversational AI for healthcare and the specific problems it helps solve.

Appointment scheduling and reminders
Conversational AI agents can handle appointment booking from start to finish: chat with patients to find the right time, provider, or location; send reminders via SMS, email, or app notifications; and process cancellations or changes in real time.
Business impact:
- Cuts front-desk workload
- Reduces no-shows and last-minute cancellations
- Improves patient satisfaction with faster access
Pre-visit patient’s intake automation
Conversational AI systems can collect basic patient information like demographics, insurance details, reason for visit, and symptoms through structured chat or voice conversations — often a smoother experience than filling out portal forms. They can also guide patients through pre-screening flows.
Business impact:
- Speeds up check-in and reduces paperwork
- Increases data accuracy by reducing manual entry
- Frees up nurses and intake staff for higher-value work
Insurance eligibility checks
Conversational AI solutions can collect insurance details like provider name, member ID, and date of birth through chat or voice. If connected to payer APIs or clearinghouses, they can run real-time eligibility checks and inform patients about coverage, co-pays, or next steps. They also handle simple exceptions — for instance, asking the patient to upload a new card if something’s missing or expired.
Business impact:
- Reduces delays in confirming coverage
- Prevents revenue loss from denied claims or unpaid visits
- Enhances patient trust by setting expectations early
Post-visit follow-up
In post-visit follow-ups, healthcare conversational AI agents can send automated check-ins like “How are you feeling after your appointment?” and gather feedback through short surveys such as NPS or satisfaction scores. It can also remind patients about medications, lab results, or next steps, like booking a follow-up with their provider.
Business impact:
- Drives better care outcomes and patient retention
- Gathers actionable feedback for service improvement
Medication reminders and refill nudges
Conversational AI can send personalized medication reminders through SMS, email, in-app chat, or even voice assistants. It can track simple responses like “Taken,” “Skipped,” or “Remind me later,” and nudge patients to refill prescriptions based on timing, dosage, or EHR data
Business impact:
- Improves adherence and reduces readmissions
- Supports chronic condition management without extra staff
Patient education and FAQ support
Conversational AI can answer common patient questions around the clock — like “What are the side effects of this medication?”, “How do I prepare for my colonoscopy?”, or “When should I follow up after surgery?” It can also provide condition-specific education in plain language, covering medicine and appointment-related topics. With the right integrations, it can personalize responses based on a patient’s visit history or symptoms, and even deliver helpful resources like PDFs, videos, or links to trusted sources.
Business impact:
- Reduces call center load and wait times
- Empowers patients with a better understanding of their care
- Improves adherence and satisfaction, especially in chronic disease management
Challenges of Implementing Conversational AI in Healthcare
The benefits of conversational AI are clear, but so are the hurdles. In healthcare, where accuracy, security, and trust are non-negotiable, even small missteps can stall adoption. Explore the most common challenges you’ll face and how to address them.

Data privacy and regulatory compliance
Non-compliance can lead to fines, lawsuits, and long-term reputational harm. Conversational AI systems process protected health information (PHI), making them subject to HIPAA, GDPR, and the EU AI Act. This means they must have enterprise-grade security measures such as end-to-end encryption, role-based access, detailed audit logs, and strict data minimization policies. When third-party LLMs or APIs are part of the workflow, it’s also essential to audit how they store, process, and retain data — including whether they train their models on it.
How to approach it:
- Map your data flows. Identify every point where PHI enters, is processed, stored, or leaves your system.
- Design for “minimum necessary” data — store only what’s essential, and keep it for the shortest possible time.
- Implement strict access control with role-based permissions, multi-factor authentication, and real-time monitoring of all logins and actions.
- Set up detailed audit logging that records every access and change to PHI, and store these logs securely for regulatory timeframes.
- Vet any third-party components (APIs, hosting, LLMs) for compliance, and run your own penetration tests to confirm claims.
The goal is to treat compliance as a continuous practice, not a one-time checkbox, so your system stays secure and audit-ready as it grows.
Integration with legacy systems
Connecting AI tools to existing healthcare infrastructure can require custom integrations, middleware, or brittle workarounds that slow deployment and drive up costs. Many organizations still depend on outdated or siloed systems that were never designed to interface with modern AI. Legacy platforms may lack APIs altogether or expose only limited functionality. Without real-time access to patient data, AI systems can’t handle high-value tasks like booking appointments, automating intake, or retrieving lab results, which sharply limits their impact.
How to approach it:
- Audit your current tech stack to map all data sources, formats, and connection points before starting AI development.
- Identify integration bottlenecks early: missing APIs, proprietary data formats, or vendor-locked databases, and factor remediation into your project timeline.
- Apply FHIR or HL7 standards where possible to normalize data exchange between systems, even if it means adding a translation layer.
- Plan for incremental integration by starting with a single, high-impact workflow (like pulling appointment availability) and expanding once the connection is stable.
- Test in a sandbox environment using realistic but de-identified data to validate performance before touching production systems.
Think of integration as infrastructure: invisible when it works, but critical to everything above it. Build it to last.
Clinical accuracy and safety
Inaccurate or misleading responses can cause harm, trigger liability, and erode patient trust. Conversational AI often handles medical questions — from symptom descriptions to post-op care instructions — which means medical content must be clinically sound, regularly reviewed, and aligned with your organization’s care standards.
How to approach it:
- Build strict escalation protocols into every workflow.
- Use clinically validated content libraries, and involve medical staff in creating and auditing responses.
If done right, clinical oversight turns AI from a risky shortcut into a safe support tool.
Bias, equity, and accessibility
AI systems don’t serve all patients equally by default. Accessibility is often an afterthought, yet it can determine whether a system truly serves everyone or silently leaves some behind. Language, literacy, culture, and socioeconomic background can all affect how patients interact with technology and how the technology responds. Models trained on narrow or biased data may misinterpret input from underrepresented groups, leading to confusion or exclusion.
Without accessible design, such as voice input, screen reader compatibility, and plain-language options, key patient populations may be left out.
How to approach it:
- Use diverse, representative training data and regularly audit AI outputs for bias.
- Design for broad accessibility — voice-first interaction, multilingual support, and clear, simple language.
- Involve patients and care teams from different backgrounds in the design process to ensure the system works for everyone, not just the digitally fluent.
The measure of success is whether every patient, regardless of background or ability, can use the system with confidence.
Staff skepticism and workflow fit
Even the best AI won’t succeed if staff don’t use it. Tools that disrupt routines or fail to align with existing workflows can create more problems than they solve. Frontline teams are already stretched thin, so anything that isn’t intuitive or well-explained will likely face pushback. When integration is poor, staff end up doing double the work, leading to frustration and ultimately the abandonment of the tool.
How to approach it:
- Involve staff early — during design, testing, and rollout.
- Focus on use cases that clearly reduce workload, like automating repetitive tasks or cutting call volumes.
- Ensure the system is transparent: show how it works, when it escalates, and how it supports clinical safety.
Adoption hinges on trust, and trust comes from clarity and collaboration.
What to Consider Before Building a Custom Conversational AI
If you're leaning toward a custom conversational AI solution — great. But before you jump in, here are a few key things to think through:
1. What problem are you actually solving?
It sounds obvious, but many teams get excited about the tech and forget the why. Are you trying to reduce call center volume? Speed up appointment handling? Streamline triage? Clarity here shapes everything — from the design to the success metrics.
2. How complex are your workflows?
Custom AI shines when you have multi-step, dynamic workflows — like verifying insurance eligibility, routing based on patient inputs, or syncing across systems. If all you need is FAQ handling, an off-the-shelf solution might be enough.
3. Do you have access to the right data?
You’ll likely need historical conversations, patient interaction logs, or structured clinical content to train or fine-tune the model. No data? You may need to start with a narrow use case while you collect it.
4. What integrations do you need?
EHRs, scheduling tools, CRM platforms — the value of conversational AI for healthcare industry multiplies when it’s integrated. If your internal systems are fragmented or hard to access, expect some extra work here.
5. Who will own it after launch?
AI isn’t a one-and-done project. It needs updates, monitoring, retraining, and governance. Decide early: Will your team maintain it? Will your vendor? Make sure someone’s steering the ship long-term.
6. Are you ready for compliance and security reviews?
If you’re in healthcare, you have to be. Think HIPAA, GDPR, SOC 2 — and, if you're in the EU, the AI Act. Building custom means you’ll have more control, but also more responsibility. Encrypt data, audit usage, and bake in transparency from the start.
Getting Started: 3 Steps to Make It Work for You
You’ve decided to invest in custom conversational AI. Now it’s time to move from idea to implementation — without overcomplicating the process.
Start small and specific
Don’t try to automate everything at once. Pick one high-impact, low-risk workflow like appointment reminders, intake Q&A, or insurance eligibility checks.
Choose a use case that is:
- Frequent enough to justify automation
- Structured enough to be reliably handled by AI
- Valuable enough to demonstrate measurable impact
2. Audit your data and integration points
Before building, make sure you can access the data your AI needs to do its job, whether that’s schedules, forms, or previous patient interactions.
Then, check what systems the AI needs to connect to. Your EHR? CRM? Billing software? The earlier you map this out, the fewer surprises you’ll hit in development.
3. Work with a partner who understands both healthcare and conversational AI
This isn’t generic chatbot work — it’s regulated, clinical, and patient-facing. Your implementation partner needs to understand:
- PHI protection and regulatory compliance (HIPAA, GDPR, EU AI Act)
- Real-world clinical workflows and patient communication norms
- The difference between a functional tool and one your staff will actually use
Look for a long-term partner, not just a dev shop. Success depends on tight collaboration, domain fluency, and a clear understanding of what’s at stake.
How Uptech Helps Apply Impactful AI Solutions in Healthcare
At Uptech, we build AI systems that are designed to work in real healthcare settings — not just in project plans or pilot environments. These solutions are developed, deployed, and integrated directly into day-to-day workflows.
Here are two examples where automation helped streamline operations and deliver measurable improvements.

Case: Medical documents processing system
In 2024, a U.S. diagnostic clinic aimed to scale patient volume while reducing admin workload. Manual document processing, like scanned reports, handwritten notes, and typed records, was slowing them down.
Uptech’s solution:
We developed a secure, HIPAA-compliant AI pipeline that digitizes, classifies, and analyzes medical documents in real time. Hosted in a private AWS cloud, the system uses OCR, NLP, and anomaly detection to automate key tasks like document tagging and classification, and detection of inconsistencies in clinical data.
Results:
- 30% reduction in document analysis time
- Thousands of staff hours saved annually
The clinic now handles growing patient volume without expanding its operations team and without sacrificing accuracy, speed, or compliance. Read more about this case here.
Case: AI-powered prescription automation solution
A digital healthcare startup in Germany aimed to simplify prescription management for patients receiving pre-packaged medications. But behind the scenes, their operations team was overwhelmed by inconsistent, manual prescription processing — with handwritten notes, mixed digital formats, and strict regulatory requirements slowing things down.
Uptech’s solution:
We built an AI-powered system that scans, decodes, and merges both handwritten and digital prescriptions into a unified medical plan. Using a multimodal LLM trained on diverse real-world data, the system handles the extraction of key fields from scanned or typed prescriptions.
Results:
- 85–90% extraction accuracy, even on handwritten input
- Reduced manual errors and smoother compliance with local standards
Discover more details in our case study.
These aren’t isolated wins, but examples of what happens when AI is implemented with precision and purpose.
At Uptech, we believe that when you target the right problems, automation can quietly take entire burdens off your team’s plate.