What is data, if not a pile of diamonds, in the era of growing AI capabilities?
Especially in healthcare, where it means an opportunity to find meaningful insights for medical research, population health, and patient care.
Yet, in this field, most of that treasure is buried, since nearly 80% of healthcare data remains unstructured, making it difficult to use to its full extent. Natural language processing (NLP) in healthcare offers a promising way forward. It can scan and transcribe documents, summarize notes, de-identify protected health information, and even surface safety signals like potential diagnostic issues.
However, it’s still just a tool — one that has to be planned, tested, and used wisely to bring real value instead of new problems.
If you’re considering NLP for your healthcare projects and want a clear view of its importance, types, and use cases, you’re in the right place.
I’m Oleh Komenchuk, ML Lead at Uptech. In recent years, I’ve worked on multiple AI projects in healthcare, and I’m happy to share the insights I’ve gained.
Specifically in this article, I’ll break down NLP in healthcare in a way that’s practical, clear, and grounded in a real-world context.
What is NLP in Healthcare?
In a medical context, NLP is a type of artificial intelligence that helps healthcare systems understand and work with human language. It is mainly used to make sense of unstructured medical information, like doctors’ notes, electronic health records, and patient feedback.
NLP in healthcare goes far beyond simply converting text into structured fields. It can organize and label information, extract key entities like diagnoses, lab results, or medications, and map them to standard medical vocabularies. It is also used to detect clinical sentiment and generate plain-language summaries so patients can better understand their care.
In practice, this means unstructured notes become searchable records, critical details surface at the right moment to support clinical decisions, routine tasks like coding and billing are automated, and complex medical language is translated into terms patients can easily follow.
Key data sources for the NLP system
For NLP to work effectively in healthcare, it needs access to a wide range of text-based information. The specific sources you prioritize should align with the business goal — for example, reducing administrative burden may require focusing on insurance claims, while improving care quality may call for analyzing clinical notes or patient feedback.
Equally important, these data sources often need preparation before NLP models can process them. This might include digitizing paper records, cleaning and standardizing text, removing duplicates, or mapping terminology to medical vocabularies like ICD-10.
Some of the most important sources include:
- Clinical notes and problem lists: progress notes, electronic health records, discharge summaries, and clinical histories that capture the patient journey.
- Imaging and pathology reports: narrative findings from radiologists and pathologists that often contain critical diagnostic details.
- Insurance claims: documentation tied to billing and coding, where accuracy directly impacts reimbursements.
- Patient messages via portals or chatbots: everyday language patients use to describe symptoms, concerns, or follow-up questions.
- Clinical research papers: scientific studies and trial reports that can feed into evidence-based decision support.
These represent the core sources, but they are not the only ones. Additional data may come from call center transcripts, wearable device reports, public health records, or even social media, depending on the scope of the project.
Together, these text streams form the backbone of NLP in healthcare, holding the insights needed for smarter operations, better patient care, and more informed decision-making
Where does NLP make a difference?
NLP is here to stay, and many healthcare organizations, including your competitors, are already adopting it to improve the way they work. If you choose to ignore it, you risk causing a strategy setback, since NLP offers proven benefits. In fact, there are three major problem areas in healthcare where NLP can make the most visible difference.
- Operational inefficiency. According to the research, physicians across all specialties spent 3.4 hours per 8 hours of scheduled patient time in the EHR during patient scheduled hours.
NLP automates the creation of structured records and makes medical histories easier to read by summarizing them on demand. This gives clinicians more time to focus on patient care.
- Clinical risk. A study by the Joint Commission found that 80% of serious medical errors stem from miscommunication during caregiver handovers: for instance, when patients transition between nurses or physicians.
NLP can scan handover reports to highlight critical details such as allergies, recent medication changes, or abnormal lab values. NLP brings key information to the surface, minimizes mistakes, and provides the full context to make safe, informed decisions during patient care.
- Financial loss. Healthcare administrative costs in the U.S. now exceed $1 trillion annually, accounting for approximately 22% of total healthcare spending.
NLP checks clinical notes for missing details, suggests the right ICD-10 or CPT codes, and automatically assembles prior authorization packets with lab results, imaging reports, and diagnoses. Basically, it offers opportunities for workflow automation, documentation accuracy, and streamlined coding that can reclaim significant financial value.
The opportunities that NLP brings will continue to expand as language-based AI becomes more embedded in healthcare. Beyond immediate gains in efficiency and accuracy, these systems provide the foundation for smarter, more connected models of care that grow along with the industry’s needs.
Most Common NLP Use Cases in Healthcare

What makes NLP stand out in healthcare is that it improves both efficiency and care quality at the same time. It speeds up back-office tasks like medical coding and prior authorizations — the approvals insurers require before certain treatments or tests — while also helping patients and clinicians with real-time documentation and plain-language communication. The examples below show some of the most important ways NLP delivers these benefits.
Automating medical coding to speed billing and reduce denials
Every time a patient visits a doctor, undergoes a procedure, or receives medication, those services must be documented in a standardized format — a medical coding, so hospitals can get paid and insurers can process claims.
These codes are the core of billing and reimbursement in healthcare. Without them, insurance companies wouldn’t know what services were provided or why they were necessary.
Traditionally, the task falls to human coders, and this manual coding process is labor-intensive and error-prone. Workers must read through lengthy clinician notes, extract the relevant details, and match them to thousands of possible codes.
Instead of relying solely on human effort, NLP systems can shoulder part of the burden, making the process faster, more accurate, and easier to manage. For example, they can:
- Scan unstructured clinician notes for mentions of diagnoses, procedures, or medications
- Suggest standardized codes automatically, with confidence scoring (a percentage indicating how certain the system is about the match), with human review serving as a safeguard to confirm the final choice
NLP doesn’t replace coders completely. However, it automates a big part of coding work, which makes the process faster and more precise.
Real-time speech-to-text for clinical documentation
Electronic health records (EHRs) have improved data storage and accessibility, but they also shifted the documentation burden onto clinicians in new ways. Unlike paper charts, EHRs require structured entry, standardized codes, and navigation through multiple screens. As a result, healthcare workers spend significant time entering or reviewing data. Sometimes it even leads to “pajama time” — after-work hours spent on notes instead of resting, which contributes to burnout and the frustration of staff.
Speech-to-text technology powered by NLP can capture conversations between healthcare workers and patients and transform them into structured EHR entries in real time. Specifically, it can:
- Generate draft notes by assembling transcribed data into a structured EHR format, ready for clinician review and approval.
- Integrate with existing workflows by syncing notes directly into the patient’s record without requiring copy-pasting or re-entry.
This use case is important since it helps to make the doctor–patient relationship more focused and reduce hours spent on EHR recordings.
Extracting structured data from doctor notes
A big part of valuable clinical information, like drug allergies or lab results, is contained in unstructured notes. Because this information isn’t captured in a structured digital format, sometimes it can’t be easily searched, analyzed, or fed into decision support tools. In some cases, it can be lost.
The true value comes from making this stream of unstructured information structured and easy to access. For doctors, it means faster access to important details that support better decisions. For administrators, it makes large-scale analysis, reporting, and forecasting possible. And for providers overall, it saves time and costs on manual entry, reduces errors, and helps increase revenue through more accurate coding and reporting.
NLP systems make unstructured data usable by:
- Scanning notes for mentions of diagnoses, medications, lab values, or staging descriptors.
- Turning doctors’ free-text notes into structured data fields that can be stored in the patient’s electronic health record (EHR) or in a research database.
With NLP, information that once required manual review becomes instantly accessible, supporting safer patient care.
For instance, a digital healthcare startup in Germany partnered with Uptech to build an AI‑powered prescription automation system. The tool uses a multimodal LLM to interpret messy, real-world prescriptions, including poor handwriting and inconsistent document formats, and consolidate them into a clean, unified medical plan with a scannable barcode. The system achieved 85–90% extraction accuracy, drastically reducing manual error and improving operational flow. Check out our case study for more information.

Converting complex documents into patient-friendly language
Healthcare documents are often written for clinicians, not patients. Medical files may be filled with medical terms hard to understand for people without a medical background. They may misinterpret or ignore instructions, leading to missed medications, delayed follow-ups, or higher readmission rates. This problem is especially relevant for patients with limited health literacy or those who don’t speak the local language fluently.
Health apps and patient portals can use NLP to automatically generate simplified explanations of medical results, giving patients accessible updates without waiting for a doctor’s call.
In this case, NLP can:
- Translate instructions into a patient’s preferred language while preserving medical accuracy.
- Automatically rewrite medical jargon into plain language that patients can understand.
- Make procedure risks and benefits clearer, improving informed consent.
When medical information is put in plain language, patients can follow their care plans more easily, stay safe during treatment, and recover better in the long run.

Streamlining prior authorizations
Before many treatments, such as an MRI or elective surgery, clinics must get approval from insurers through a process called prior authorization. This requires staff to gather evidence that the patient actually needs specific treatment across their record: lab results, imaging reports, physician notes, and documented diagnoses.
Usually, this is a manual and time-consuming process. Staff may spend 2–3 days to pull information from scattered sources, format it for insurer requirements, and double-check for completeness. Delays frustrate patients, slow down care, and increase administrative costs for providers.
NLP can automate much of this work by:
- Extracting relevant information from across the EHR.
- Assembling insurer packets automatically, formatting the information into standardized forms required by payers.
- Flagging missing documentation so staff can address gaps before submission.
A practical example comes from a U.S. diagnostic clinic that partnered with Uptech to build a medical document processing system. By combining OCR with NLP, the clinic was able to digitize handwritten notes, extract structured medical data, and classify documents reliably. The result was a 30–34% reduction in analysis time, saving thousands of staff-hours annually and nearly doubling monthly patient capacity. Explore all the details in our case study.
Basically, NLP removes one of telehealth’s biggest barriers: documentation overload. Providers get accurate notes instantly, patients benefit from more attentive virtual visits, and health systems gain long-term insights from consistent data capture across remote care.
Challenges of Implementing NLP in Healthcare
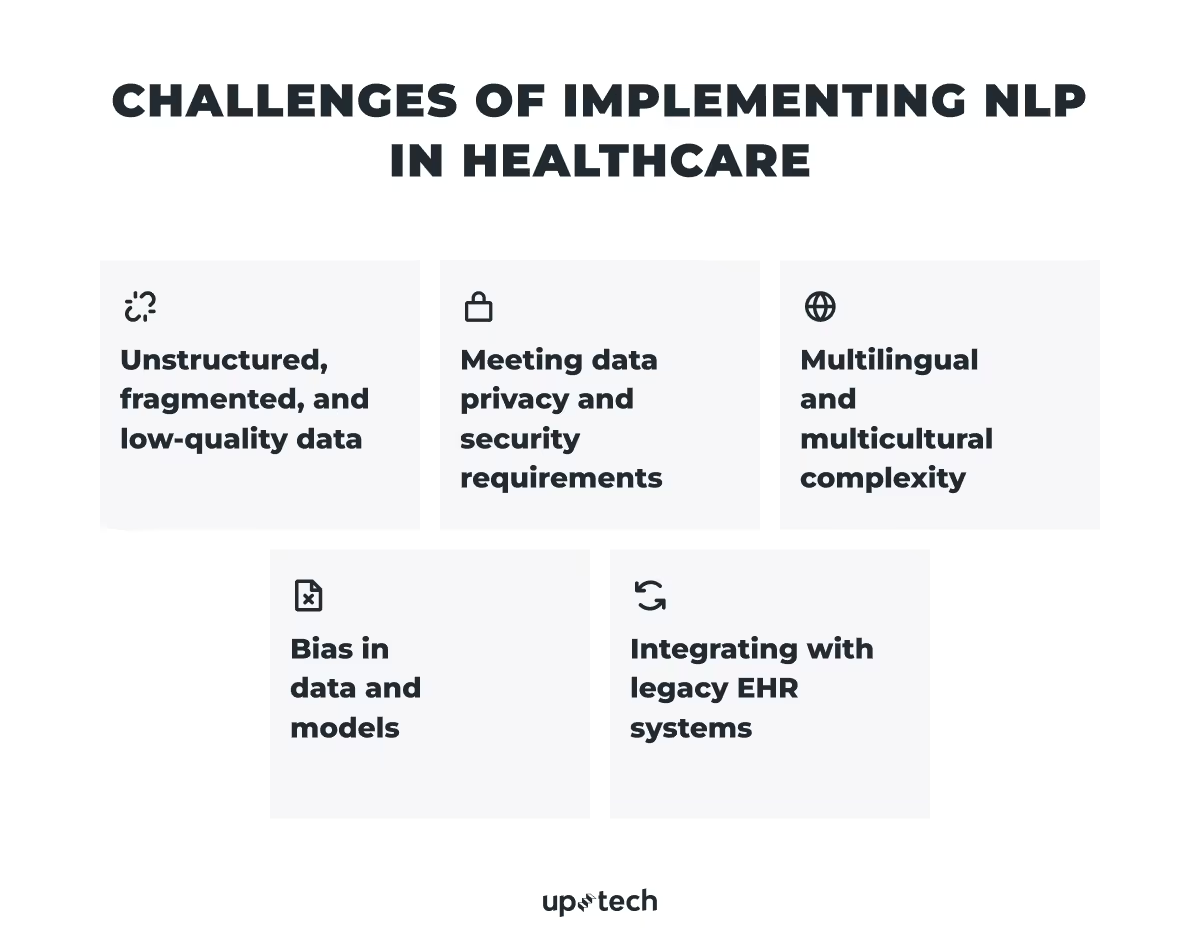
NLP holds great promise for healthcare, but putting it to work in real-world scenarios isn’t easy. Medical data is sensitive, scattered across systems, and varies a lot between patients. And unlike most industries, mistakes here carry serious risks. Below are the biggest challenges and practical ways to address them.
Unstructured, fragmented, and low-quality data
Clinical data exists in many forms: free-text notes, scanned PDFs, dropdown fields, images, and even voice recordings. Documentation styles vary widely between providers, with inconsistent language, abbreviations, and shorthand. Training NLP models on this “dirty” data can lead to poor accuracy, misleading outputs, and loss of clinician trust.
What’s the solution?
To make messy clinical data usable, healthcare organizations can invest in preprocessing and normalization pipelines. Scanned documents and faxes, for example, are passed through optical character recognition so they can be read as text rather than images. Free-text notes are segmented into meaningful sections, such as patient history, findings, and impression, so models can focus on the right context. Sensitive details like patient names or addresses are routinely stripped out through de-identification, ensuring compliance and allowing the data to be used safely for model training.
Also, because no amount of automation can account for every nuance, clinicians need to be kept in the loop. They can validate extracted data before deployment and provide ongoing feedback, which helps refine model accuracy in real-world use. Over time, this human oversight ensures that the system not only functions technically but also aligns with the realities of clinical practice.
Meeting data privacy and security requirements (HIPAA/GDPR)
Because NLP systems process medical records, they inevitably handle highly sensitive patient data. Regulations such as HIPAA in the U.S. and GDPR in the EU set strict rules for how this information must be stored, accessed, and shared. Even a single oversight can result in fines, legal action, and long-term reputational damage. For healthcare organizations, the stakes are not just financial but ethical: maintaining patient trust depends on airtight data protection.
What’s the solution?
To avoid risk, most organizations can build multiple layers of security around their NLP systems. Patient records should be stripped of identifiers before being used for model training, and when identifiable data must be processed, it needs to be protected with strong encryption protocols.
Equally critical is the infrastructure itself. Hospitals and vendors increasingly rely on HIPAA- and GDPR-compliant cloud platforms or on-premises servers certified to handle medical data securely. Beyond the technical safeguards, compliance is treated as an ongoing process: periodic audits, penetration tests, and policy reviews help catch gaps before regulators or attackers do.

Multilingual and multicultural complexity
Healthcare rarely happens in a single language. Large health systems serve diverse populations where clinical notes, patient queries, and even lab reports can appear in multiple languages, regional dialects, or with culturally specific terminology. For example, a Spanish-speaking patient might describe chest pain differently than an English-speaking one, or a clinician in Eastern Europe might use shorthand unfamiliar to models trained on U.S. datasets. Standard NLP models, which are often trained primarily on English-language corpora, struggle in these settings, leading to lower accuracy, missed extractions, and a risk of inequitable care.
What’s the solution?
To bridge the gap, organizations can adopt multilingual or domain-adapted models that process more than one language while recognizing medical context. Training datasets are curated to include examples from local patient populations, capturing the way symptoms, conditions, or treatments are actually described in that region. This way, the system recognizes both the formal clinical language and the colloquial ways patients report their health.
Equally important is human involvement. Bilingual clinicians often play a key role in validating outputs, correcting mistranslations, and highlighting cultural nuances that a model might miss. For instance, a phrase common in one community carries a different medical implication elsewhere. Over time, this combination of multilingual training and human refinement allows NLP systems to better reflect the linguistic and cultural realities of the populations they serve.
Bias in data and models
Healthcare data is not neutral. Decades of clinical practice and record-keeping reflect existing inequities in access, diagnosis, and treatment across gender, race, and socioeconomic status. For instance, women’s symptoms of heart disease are often under-documented compared to men’s, and minority populations may have less complete medical histories due to barriers in access. When medical natural language processing systems are trained on these datasets, they risk learning and reproducing those same biases.
What’s the solution?
To counteract this, organizations increasingly treat bias detection and mitigation as core steps in NLP development. Training datasets are diversified to include records from different demographic groups, regions, and clinical specialties, ensuring the system isn’t overfitted to one population. During development, teams run fairness and bias audits, systematically checking whether the model performs equally well across gender, age, or ethnic subgroups.
Integrating with legacy EHR systems without workflow disruption
Electronic health record (EHR) systems are the backbone of modern healthcare, but many in use today were built before AI or NLP tools were introduced. These legacy systems often lack flexible architectures or standardized APIs, making integration difficult. If NLP is integrated poorly, it can slow system performance, introduce duplicate data entry, or force clinicians to jump between multiple screens. In an environment where every extra click adds to frustration and burnout, such inefficiencies can quickly undermine adoption, even if the underlying technology is powerful.
What’s the solution?
The most common way to link modern medical natural language processing tools with older EHRs is through middleware and FHIR-based connectors.
Middleware acts as a translator between the EHR and the AI tool. It reformats data so the AI can process it, then sends outputs like codes, summaries, or alerts back into the EHR in the right format. Along the way, it also manages security, access, and error handling. The benefit: no need to rebuild the EHR from scratch — middleware simply plugs in and makes communication possible.
FHIR (Fast Healthcare Interoperability Resources) provides a common data standard. A FHIR connector uses this standard to ensure patient data always looks consistent across systems. That consistency makes it easier to add or swap AI/NLP tools without custom integrations each time.
Together, middleware and FHIR connectors create a seamless bridge between legacy EHRs and modern AI. For clinicians, this means AI insights appear naturally in their workflow, without extra clicks or screen-hopping.
Best Practices for Implementing NLP in Healthcare
For healthcare leaders, clinicians, and innovators exploring NLP, the main takeaway is clear: the technology holds enormous potential, but its success depends on careful implementation. Even if you’re not planning to build NLP systems today, understanding the principles that guide effective adoption can help you prepare for what comes next.
Here are a few best practices most healthcare organizations follow when moving from pilots to real-world use.
Define ground truth with clinician consensus
A model is only as good as its labels. In healthcare, “ground truth” can vary (for example, one physician codes “chest pain” as a symptom, another as a condition). Run calibration workshops with 5–10 clinicians to align definitions before annotation — it prevents months of retraining later.
Measure success with dual KPIs
Accuracy metrics such as precision, recall, and F1 score show how often the model correctly identifies or misses important medical terms. They are necessary, but not enough on their own.
In healthcare, a model can achieve excellent technical scores yet still fail in practice if it slows clinicians down or doesn’t fit their workflow. That’s why you also need clinical adoption metrics: reduction in EHR clicks, minutes saved per patient encounter, or error rate reduction in billing. Optimizing for both ensures the system is not only accurate on paper but also usable and valuable in daily care.
Plan for model update like you plan for audits
Medical language doesn’t stand still. New treatments, revised coding standards, and unforeseen events can quickly make yesterday’s terminology outdated. Left unchecked, this drift chips away at an NLP system’s accuracy. The fix is to approach updates with the same discipline as regulatory audits. Just like compliance teams plan HIPAA or GDPR reviews, AI teams should schedule checkpoints to re-evaluate the model with new data, update vocabularies, and retrain when needed. This keeps performance steady and aligned with real-world practice.
NLP in healthcare is about building trust, protecting patients, and improving workflows step by step. For now, the most important thing is awareness: knowing where NLP can add value and what challenges lie ahead. That way, when the time comes to adopt or invest, you’ll be prepared to move forward confidently.
At Uptech, we help healthcare companies turn unstructured data into practical systems. If you’re considering implementing NLP in your healthcare project and want to explore what’s possible, book a free consultation with our team — we’ll walk you through potential use cases and outline a clear, actionable path forward.