Many leaders are trying to understand what comes next and which healthcare trends will matter most in 2026.
Healthcare is changing along with society. Medicine is now closely connected to technology and AI. At the same time, healthcare is becoming more personal and focused on individual needs.
The global healthtech market is expected to reach $3.1 trillion by 2033. The numbers show how big this change really is.
According to McKinsey, 85% of healthcare leaders are already using generative AI or actively exploring it.
Today, AI is used in less than 15% of the global healthcare market. By 2030, this number is expected to grow to more than 30%.
These stats give a good general picture of the major market shifts. But they don’t answer the most important question: which trends should you focus on to make better business decisions?
I’m Yan Likarenko, a product manager at Uptech, and below are the healthcare trends I believe will shape the near future.
Let’s get started.

1. AI becomes operational infrastructure
AI is no longer a side project owned by innovation teams. It gradually becomes operational infrastructure.
That happens because healthcare faces compounding operational stress. Documentation and inbox burden continue to consume clinician time and attention. Revenue cycle complexity rises (coding rules, prior authorization, denials, documentation requirements). Patient complexity increases (multi-morbidity, polypharmacy, fragmented histories). Workforce shortages limit how much human capacity you can add, even if you have a budget.
So AI becomes a workforce stabilizer and throughput engine.
- 65% of U.S. healthcare organizations already say AI is transforming their operations, especially admin workflows and clinical support.
- Deloitte estimates gen AI and automation can halve revenue-cycle admin time and free up ~20% of nurses’ time for direct care.
- HHS (US) recently published a federal AI strategy to scale AI across public health and patient care.
What changes in 2026:
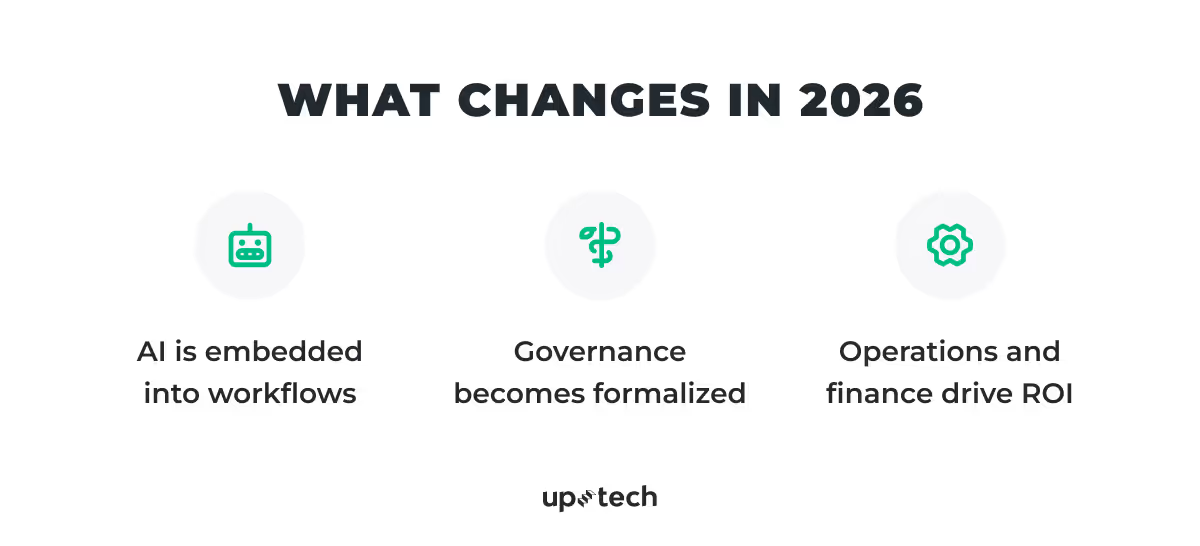
AI is embedded into workflows
Ambient documentation, coding support, and clinical note generation is embedded directly into major EHRs and practice-management platforms. Not as optional pilots or bolt-on tools, but as standard features. Clinicians won’t “open an AI app.” AI will simply be part of how the EHR works.
Governance becomes formalized
Hospitals will introduce AI governance structures, often referred to as AI formularies, similar to drug formularies. These committees will decide which models are approved, where they can be used, what data they can access, and how they’re monitored. The logic is clear: like medication, AI delivers value but carries risk, and it requires structured oversight.
Operations and finance drive ROI
A growing share of AI’s impact concentrates in system-level workflows such as revenue cycle management, utilization review, quality reporting, and clinical documentation integrity. These applications improve accuracy, reduce delays, and lower administrative friction at scale. The key shift is not visibility, but economics: AI delivers its strongest returns where performance is measurable, governable, and repeatable across the organization.
Strategic angle for healthtech builders
In 2026, “we use AI” will be assumed. It won’t influence buying decisions.
What will matter is how well AI is executed in real healthcare environments.
- Embed AI directly into existing workflows. Solutions should operate inside EHRs, revenue-cycle systems, and care coordination tools. If clinicians need to switch contexts or learn new routines, adoption will stall.
- Treat governance and transparency as product features. Be explicit about data access, model behavior, human oversight, and monitoring. Buyers will expect clear answers upfront, not after procurement begins.
- Anchor value in operational metrics. AI must demonstrate impact in terms of healthcare operators already measure: clinician time saved, denials reduced, billing cycles shortened, and throughput improved. Narrative value won’t scale; measurable outcomes will.
Winning products will feel invisible but indispensable — safely embedded, easy to govern, and economically obvious inside systems healthcare teams already rely on.

2. Telemedicine becomes structural
Telemedicine is becoming a permanent layer of healthcare delivery.
The first wave of virtual care was driven by necessity. What keeps it in place now is economics, capacity, and patient behavior. Health systems are under pressure to do more with the same, or fewer, resources. Clinician shortages persist. Physical locations are expensive to scale. And patients have learned that many interactions do not require a clinic visit.
At the same time, care itself has changed. Chronic disease management, behavioral health, post-acute follow-ups, medication management, and triage are fundamentally communication-heavy. They benefit more from continuity and responsiveness than from physical presence.
So, telemedicine evolves from “remote visits” into a coordination layer for care delivery.
Telemedicine will shift from replacing in-person care to deciding when in-person care is actually necessary.
What changes in 2026
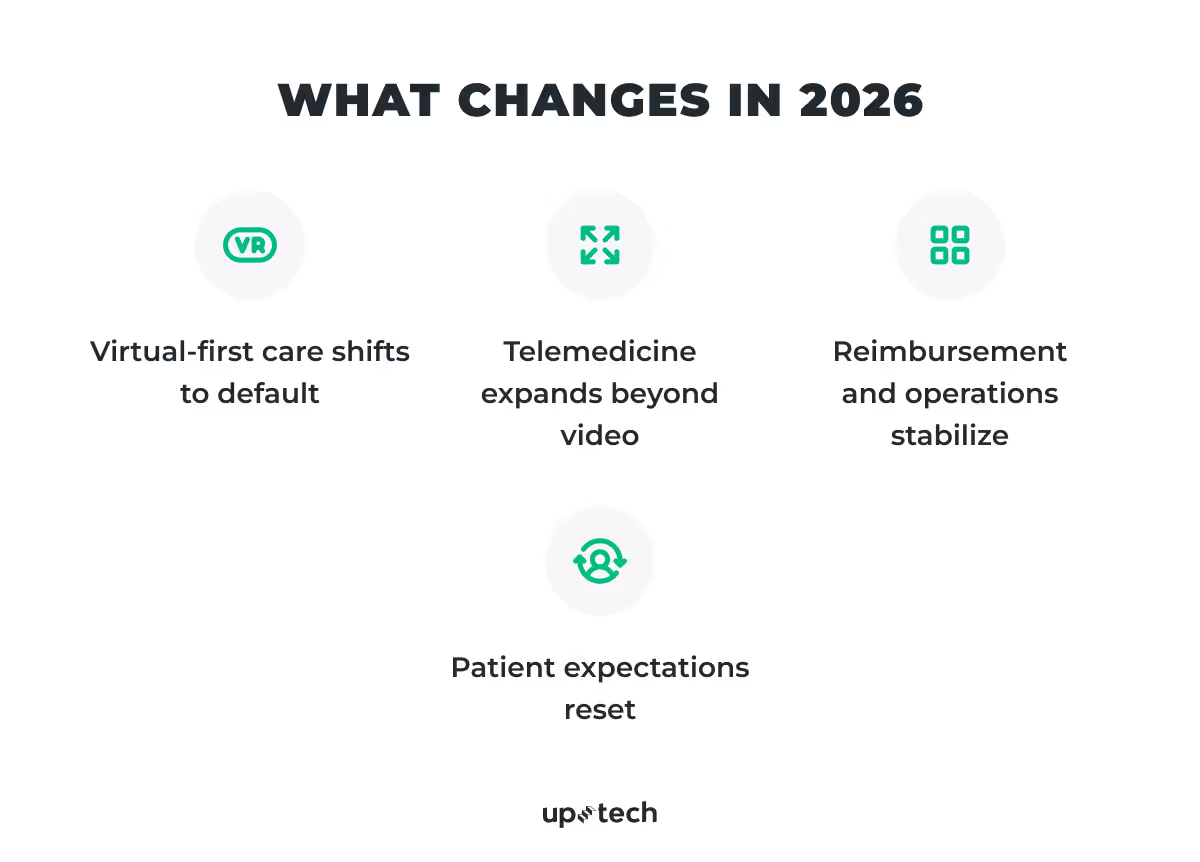
Virtual-first care shifts to default
For many conditions, the first point of contact will become virtual by default. In-person visits are reserved for procedures, diagnostics, and complex examinations. This reverses the traditional flow of care and reduces unnecessary utilization while preserving clinical quality.
Telemedicine expands beyond video
Video calls alone are no longer the product. Telemedicine now spans asynchronous messaging, digital intake, follow-ups, care coordination, and remote lab testing as part of a continuous care loop.
In one of the projects we worked on, MicroGenDX, virtual care was paired with at-home diagnostics. Clinicians reviewed lab results, communicated next steps, and adjusted treatment remotely, reducing delays and unnecessary in-person visits.
The value of telemedicine now comes from continuity across touchpoints, not from the video call itself.
Reimbursement and operations stabilize
Payers will move from temporary telehealth policies to more predictable reimbursement frameworks. Health systems design workflows assuming virtual care will remain, rather than treating it as an exception. Operational planning finally catches up with patient behavior.
Patient expectations reset
Patients now expect convenience, fast access, and minimal friction. Virtual care will become part of the baseline experience, especially for mental health, chronic care, and routine follow-ups. Products that treat telemedicine as a secondary feature will start to feel outdated.
Strategic angle for healthtech builders
Offering “telemedicine features” won’t be enough.
Healthtech teams should focus on making virtual care operationally indispensable.
- Design virtual care around clinical workflows, not visits. Telemedicine should support triage, follow-ups, chronic care, and coordination without forcing clinicians to manage parallel processes.
- Integrate deeply with core systems. Seamless connections to EHRs, scheduling, billing, and care teams are essential. Fragmented virtual care increases operational burden rather than reducing it.
- Prove impact on capacity and cost. Virtual care must reliably reduce wait times, clinician load, and unnecessary in-person visits, with outcomes measured across hybrid care journeys.
3. Data-driven decision support reshapes care delivery
One of the most underestimated shifts in healthcare is the evolution of clinical reasoning itself.
Healthcare produces more data than clinicians can realistically process. Lab results, imaging, clinical notes, genomics, device data, and long longitudinal histories all compete for attention. AI-driven analysis increasingly works as a cognitive extension. It does not make decisions, but it shapes how information is organized, prioritized, and presented.
In practice, clinical decision support most often helps by:
- Highlighting abnormal patterns across time rather than isolated values
- Surfacing relevant prior cases and cohort-level context
- Summarizing complex histories into clear, actionable views
- Suggesting possible differential diagnoses or next diagnostic steps
In one of the projects we worked on, an AI-powered medical image processing system supported clinicians by analyzing imaging data, flagging relevant patterns, and reducing manual review effort. The system did not replace clinical judgment, but helped clinicians focus attention where it mattered most.
These tools are built to assist, not to replace clinical judgment. Both regulation and clinical culture reinforce that responsibility and accountability remain with the clinician.
What changes in 2026
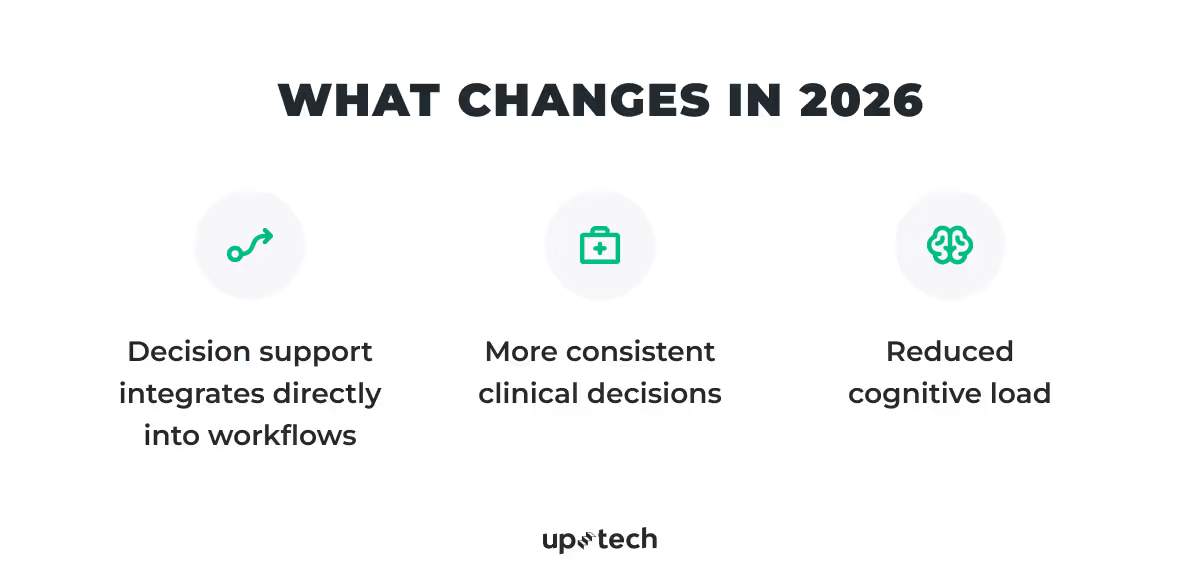
Decision support integrates directly into workflows
Analytical insights are delivered inside EHR and clinical systems rather than through separate tools or dashboards. Longitudinal data is analyzed continuously, enabling earlier detection of deterioration, risk, or deviation from expected trajectories. Clinicians receive clearer signal without additional workflow steps.
More consistent clinical decisions
As decision support tools mature, variability driven by information overload and fragmented histories decreases. Care becomes more standardized across providers and sites, not because judgment is constrained, but because relevant context is surfaced more reliably at the point of decision.
Reduced cognitive load
The role of the clinician does not change. Decision rights remain human, but clinicians operate with better context, fewer blind spots, and less mental overhead. AI supports reasoning under pressure rather than introducing new complexity.
Strategic angle for healthtech builders
AI-driven insights alone are not a differentiator. What matters is how those insights are delivered and used in practice.
- Make reasoning transparent and explainable. Clinicians must be able to understand why an insight appears and how it was generated. Opaque recommendations will be ignored, regardless of accuracy.
- Reduce risk and cognitive load at scale. Winning systems consistently surface relevant signals, reduce missed risk, and limit unwarranted variation without overwhelming clinicians.
In 2026, AI-assisted decision support will be expected to operate as a reliable cognitive layer within everyday care delivery.
4. Precision and predictive care scale
For years, precision medicine lived at the edges of care. Genomics, advanced imaging, and predictive models were powerful, but mostly confined to research settings, specialty centers, or narrow use cases. In 2026, that will begin to change.
What moves precision care forward is not a single breakthrough, but the convergence of data sources. Clinical records, genomics, imaging, biomarkers, device data, and patient-reported outcomes are increasingly analyzed together. This multimodal view allows risk to be assessed earlier, care to be tailored more precisely, and interventions to be timed before deterioration occurs.
Importantly, this does not mean fully individualized care for every patient. Instead, precision shows up where it delivers clear clinical and economic value.
What changes in 2026
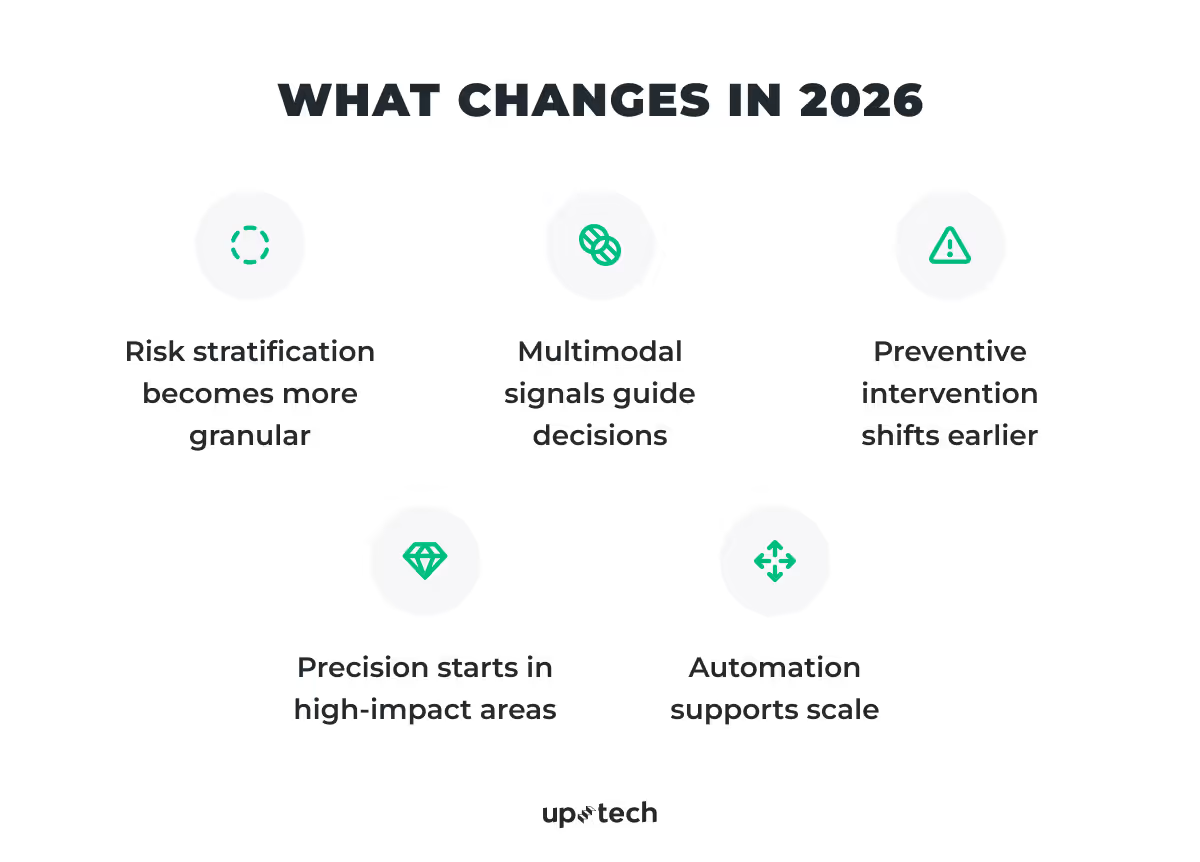
Risk stratification becomes more granular
Predictive models segment patient populations beyond simple rules or averages. Health systems identify who is likely to deteriorate, be readmitted, or fail therapy earlier, allowing targeted intervention rather than blanket programs.
Multimodal signals guide decisions
Genomics, imaging-derived features, lab trends, and device data are combined to support specific decisions, such as therapy selection, monitoring intensity, or escalation timing. These insights are embedded into workflows, not presented as standalone analytics.
Preventive intervention shifts earlier
Predictive insights support earlier outreach, medication adjustments, and care plan changes before acute events occur. This is especially visible in oncology, cardiology, and chronic disease management.
Precision starts in high-impact areas
Early routine adoption concentrates in areas with strong evidence and reimbursement alignment, including oncology, cardiology, rare disease pathways, and population health management.
Automation supports scale
AI-driven analysis enables precision approaches to operate across thousands of patients, not just a few complex cases, without overwhelming clinicians.
Strategic angle for healthtech builders
Precision is not measured by model sophistication, but by clinical impact.
What differentiates products is whether predictive insights improve decisions at the point of care.
- Tie multimodal insights to specific clinical actions. Predictions must clearly inform what changes next: outreach, monitoring intensity, therapy choice, or escalation timing.
- Prove impact where it matters. Successful platforms demonstrate measurable improvements in outcomes, utilization, or cost, not just model performance.
Precision and predictive care will not replace standard medicine. They will quietly shift decisions earlier, enabling timely intervention while preserving clinical judgment.
5. Health consumerization
Healthcare will increasingly be shaped by consumer expectations set outside the industry. Patients will compare healthcare experiences not to other hospitals, but to banking apps, marketplaces, and everyday digital services.
This shift will often be labeled “consumerization,” but the real change will be structural. Healthcare interactions will consolidate into platform-like ecosystems that organize services, data, and communication in one place. Instead of fragmented portals and point solutions, patients will increasingly engage through a single digital front door.
What will change in 2026
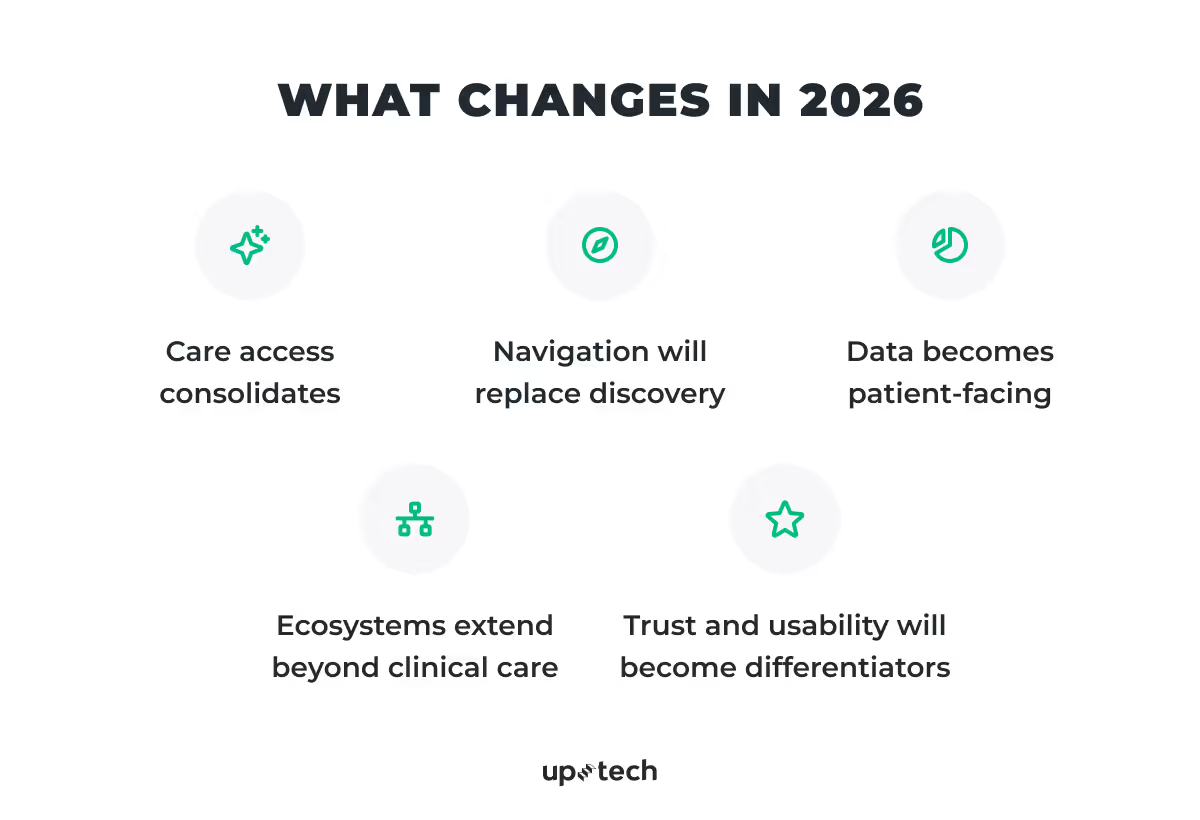
Care access consolidates
Patients will manage appointments, virtual visits, prescriptions, lab results, payments, and follow-ups within one interface. The goal will not be feature density, but continuity and reduced friction across the care journey.
Navigation will replace discovery
Health systems will move away from making patients search for services. Digital platforms will guide users to the right care level based on symptoms, history, and eligibility, reducing unnecessary visits and misrouted demand.
Data becomes patient-facing
Clinical data, device inputs, and patient-reported information will be surfaced in coherent, understandable views. This will support adherence, self-management, and ongoing engagement between encounters.
Ecosystems extend beyond clinical care
Super-apps will increasingly integrate wellness, mental health, pharmacy, insurance, and employer benefits. This will reflect how patients experience health as a continuous part of daily life rather than isolated clinical events.
Trust and usability become differentiators
As platforms consolidate touchpoints, clarity, privacy, and intuitive design will matter as much as functionality. Poor UX or unclear data use will erode trust quickly at scale.
Strategic angle for healthtech builders
Patient-centered language is easy; patient retention is not.
What matters is whether patients return to the product as part of their care routine.
- Own a clear moment of value. Successful platforms focus on a meaningful part of the journey: access, navigation, adherence, or ongoing engagement, rather than shipping isolated features.
- Prioritize simplicity and trust. Experiences must be intuitive, reliable, and respectful of patient data. Products patients understand and return to will outperform those that merely add functionality.
Health consumerization will reward platforms that reduce friction, build trust, and become a natural part of patients’ everyday health interactions.
6. Governance, security, and trust become key filters
Governance, security, and trust will serve as hard filters, determining which technologies can be adopted and scaled in healthcare.
As AI, data sharing, and digital platforms become embedded into core operations, risk exposure will increase. Health systems will operate in an environment of heightened regulatory scrutiny, public sensitivity around data use, and low tolerance for failure. In this context, technical capability alone will not be enough.

What will change in 2026
Formalized AI and digital governance
Health systems will introduce clearer structures for approving, monitoring, and retiring digital tools and AI models. Decision rights, escalation paths, auditability, and model oversight will be defined upfront rather than handled reactively.
Security goes beyond compliance
Meeting baseline requirements such as HIPAA or GDPR will be assumed. Buyers will expect demonstrable security practices, continuous monitoring, and clear incident-response processes. Security posture will be evaluated as an ongoing capability, not a checkbox.
Trust becomes prerequisite
Clinicians and patients will expect clarity around how data is used, how models behave, and where human oversight applies. Solutions that cannot explain their behavior or data flows will struggle to gain acceptance, regardless of performance.
Transparency shapes perception
As AI becomes more visible in care delivery, communication around safeguards, limitations, and accountability will matter. Poor transparency will translate quickly into reputational and regulatory risk.
Strategic angle for healthtech builders
As digital systems move into the core of healthcare operations, governance becomes decisive.
- Design for governance from the start. Build auditability, oversight, and clear decision rights into the product rather than treating them as add-ons.
- Treat security as a continuous practice. Move beyond certifications toward ongoing monitoring, testing, and incident readiness.
- Communicate transparently. Make data use, access, and model behavior understandable to clinical, legal, and executive stakeholders.
In 2026, products that are easy to govern will be the ones that scale.

Final perspective
From an expert standpoint, the most accurate description of healthcare in 2026 is operationally mature, digitally dependent, and cautiously progressive.
Telemedicine becomes the default entry point for many care journeys. AI supports clinicians through analysis, documentation, and coordination rather than autonomous decision-making. Data is used earlier, more responsibly, and more predictively.
The system does not become fully automated. Instead, it becomes more human by removing friction, reducing overload, and allowing clinicians to focus on judgment, empathy, and complex care.
In 2026, the organizations that succeed are not the most experimental, but the ones that integrate technology quietly, safely, and deeply into everyday care delivery.