Today, healthcare is moving toward convenient, on-demand access — care that fits people’s lives, not the other way around. From patients with mobility challenges to those in rural areas or packed schedules, digital health is making medical help more accessible than ever.
What once felt innovative is now becoming the standard. To stay competitive, many healthcare organisations are already using or planning to use digital tools.
One of the most impactful among them is the doctor-on-demand app. Building a doctor-on-demand app helps providers reach more patients, offer more personalised care, and speed up service delivery. It’s also a promising area for business growth.
According to Grand View Research, the global telehealth market is expected to reach USD 455.27 billion by 2030, creating significant opportunities for companies that move early.
If you’re thinking about developing your own doctor-on-demand app, this guide will walk you through the main stages, benefits, and key things to consider. As a product manager who has worked on several healthtech projects, I’ll share my professional insights to help you move faster and smarter.
Let’s get started.
What Is a Doctor On-Demand App?
A doctor-on-demand app is a telehealth service that provides 24/7 virtual access to certified doctors via secure video visits on a phone, tablet, or computer.
Such apps help users to get treatment for common, non-emergency health issues or receive needed medical prescriptions. They also often offer mental health support for conditions like anxiety and depression, and can provide doctor's notes for work or school.
Why Companies Build Doctor On-Demand Apps
Doctor on-demand–style apps represent a new era of care delivery, where convenience, personalization, and data work together to create better health outcomes and stronger financial performance. Companies across healthcare, insurance, and even corporate wellness are investing in these platforms not just to keep up with trends, but to build entirely new value channels.
Expanded reach to the customer base
One of the main reasons telehealth has grown so fast is accessibility. A doctor-on-demand app removes geographical limits and lets patients consult licensed healthcare professionals from anywhere, whether they live in a large city or a remote village.
With a well-designed telehealth solution, healthcare organizations can treat patients far beyond their local area: across cities, regions, or even countries (depending on licensing). This approach works especially well for companies that aim to:
- Reach underserved or rural populations. Many communities still lack access to qualified specialists. Through a virtual platform, patients in remote areas can meet top professionals within minutes. This expansion grows the patient base and positions the brand as one that values accessibility and social responsibility.
- Offer care around the clock. When doctors or partner specialists work in different time zones, the platform can stay available 24/7 without exhausting a single team. This setup improves patient satisfaction and helps smaller providers compete with large telehealth platforms that promise instant access.
- Scale without physical expansion. Digital scalability enables organizations to increase service capacity without opening new clinics, hiring reception staff, or leasing additional facilities. Each licensed provider added to the system broadens overall service coverage, making telehealth one of the most cost-efficient growth mechanisms in modern healthcare.
- Build a multi-regional or global presence. For startups and private practices alike, geography no longer limits growth. Once compliance and licensing rules are met, a telehealth app can operate across regions as a trusted virtual clinic beyond physical borders.
In the end, expanding reach through telehealth means scaling care like a tech company, not a hospital. It lets you grow access, efficiency, and brand visibility at the same time without limits of walls or zip codes.
Multiple revenue models
Doctor on-demand apps open the door to flexible, scalable monetization strategies that fit different business models:
- Per-consultation fees or commission-based models for individual providers or marketplaces.
- Subscription or membership plans that provide a steady recurring income.
- Corporate wellness partnerships, where companies pay for employee access.
- White-label licensing — reselling the app’s infrastructure to other healthcare organizations.
This diversification helps reduce reliance on traditional, location-bound income streams and builds resilience against market fluctuations.
Reputation and long-term brand equity
Digital convenience is now a basic expectation across every industry. People who handle their banking, shopping, and travel online also expect the same speed and ease from healthcare. Organizations that provide simple, on-demand medical services come across as responsive, modern, and patient-focused — qualities that are now part of what patients define as true clinical excellence.
Every positive interaction within the app becomes part of the brand narrative. As telehealth adoption normalizes, organizations that established digital credibility early will hold a distinct competitive advantage. Their names become associated not only with clinical reliability but with effortless, patient-first innovation.
In essence, telehealth functionality strengthens brand equity on two fronts:
- Externally, by improving visibility, reputation, and patient trust.
- Internally, by fostering a culture of digital competence and service excellence.
The result is a healthcare brand perceived as both caring and technologically mature, which is the precise balance modern patients and partners seek.

Core Features of a Doctor on Demand App
A doctor-on-demand platform brings together three main user groups: patients, doctors, and administrators, within one secure and unified digital space. Each group needs a specific set of features that provide accessibility and efficiency.

Below is a breakdown of the core functionality and the purpose behind each feature.
Patient-side features
Patients are the core users of any telehealth app, and their expectations now mirror those set by consumer technology: simplicity, speed, and transparency. The following features are essential for creating a smooth patient journey.
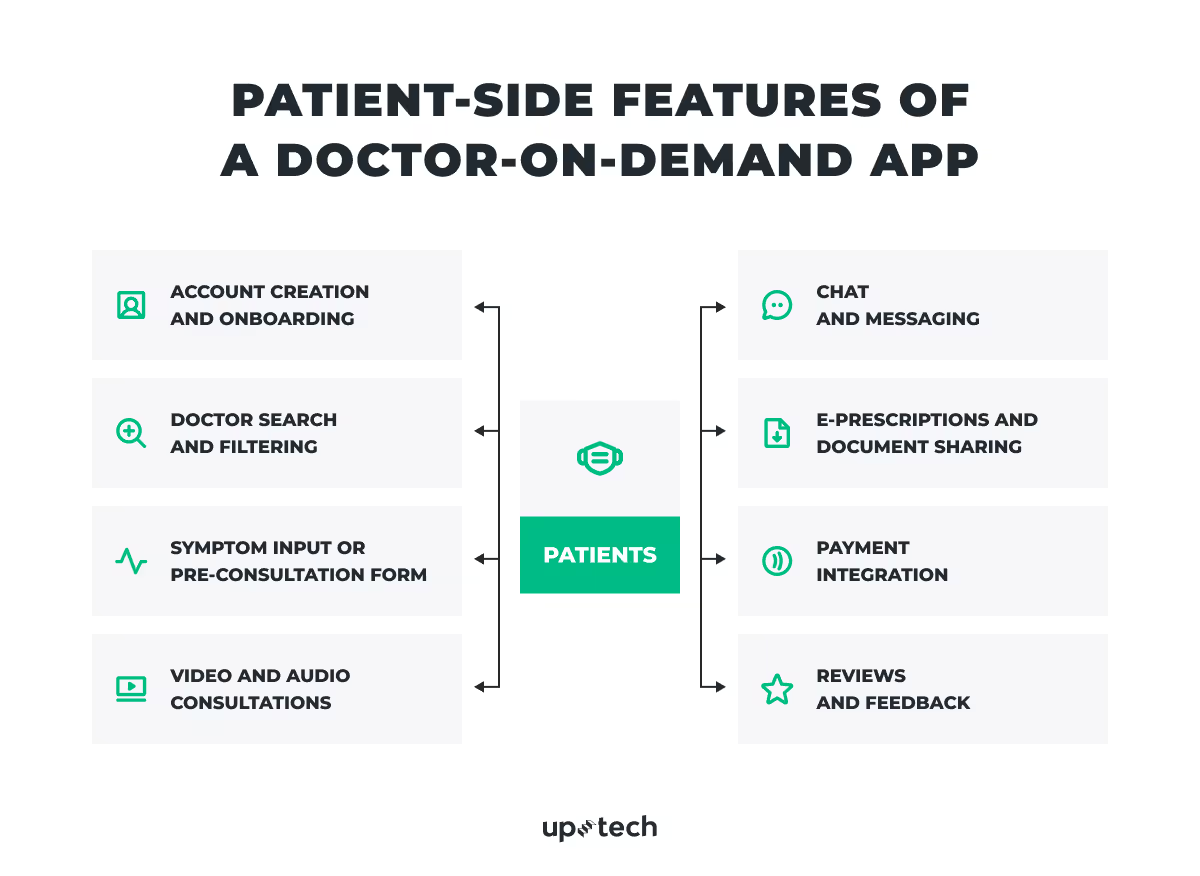
Account creation and onboarding
Patients should be able to register quickly via email, phone, or social login, with secure identity verification. A short onboarding flow explains how to find doctors, book visits, and access prescriptions.
Doctor search and filtering
A structured search with filters for specialty, language, rating, price, or availability helps patients find the right doctor instantly. Adding AI-powered suggestions can make results even more relevant.
Symptom input or pre-consultation form
A short intake form lets patients describe symptoms, upload files, or share test results before the visit. This saves time during the consultation and helps doctors prepare in advance.
Video and audio consultations
High-quality video calls form the heart of the experience. A stable, low-latency connection keeps communication smooth, while options like screen sharing or document notes make the consultation more interactive.
Chat and messaging
Secure in-app chat allows patients to ask quick questions, get follow-up instructions, or share files without booking another visit. End-to-end encryption protects privacy and ensures continuity of care.
E-prescriptions and document sharing
After a session, doctors can issue digital prescriptions or upload medical notes that patients can view, download, or forward to a pharmacy.
Payment integration
A built-in payment system (for example, Stripe, PayPal, or Braintree) enables patients to pay directly in the app. Clear pricing and instant receipts build trust and make the process smoother.
Reviews and feedback
Ratings and reviews improve transparency, help other patients choose with confidence, and give the platform insight into service quality and doctor performance.
Doctor-side features
For medical professionals, the app should simplify scheduling, documentation, and communication while giving full control over daily workflows.

Profile management
Doctors can create detailed profiles that include their specialization, qualifications, certifications, and consultation fees
Scheduling and availability management
An easy-to-use calendar lets doctors set consultation hours, approve or decline bookings, and handle cancellations. Real-time updates prevent double bookings and help minimize patient wait times.
Electronic health record (EHR) access
Secure access to patient data and visit history supports informed, consistent care. Integration with existing EHR systems such as Epic, Cerner, or Allscripts enables seamless data exchange across platforms.
Consultation management
Doctors can start video calls, review patient files, take notes during the session, and store consultation summaries directly within the app.
Billing and payouts
Automatic invoice generation and transparent payout tracking make it easier for doctors to monitor earnings and cut down on administrative work.
In-app communication
Encrypted chat allows secure post-visit communication between doctors and patients without revealing personal contact details.
Analytics dashboard
Visual summaries showing patient volume, consultation trends, and satisfaction scores give doctors valuable insights to refine their services and grow professionally.
Administrator-side features
Administrators are the operational backbone of a telehealth platform. They maintain system stability, ensure compliance, and oversee financial integrity.
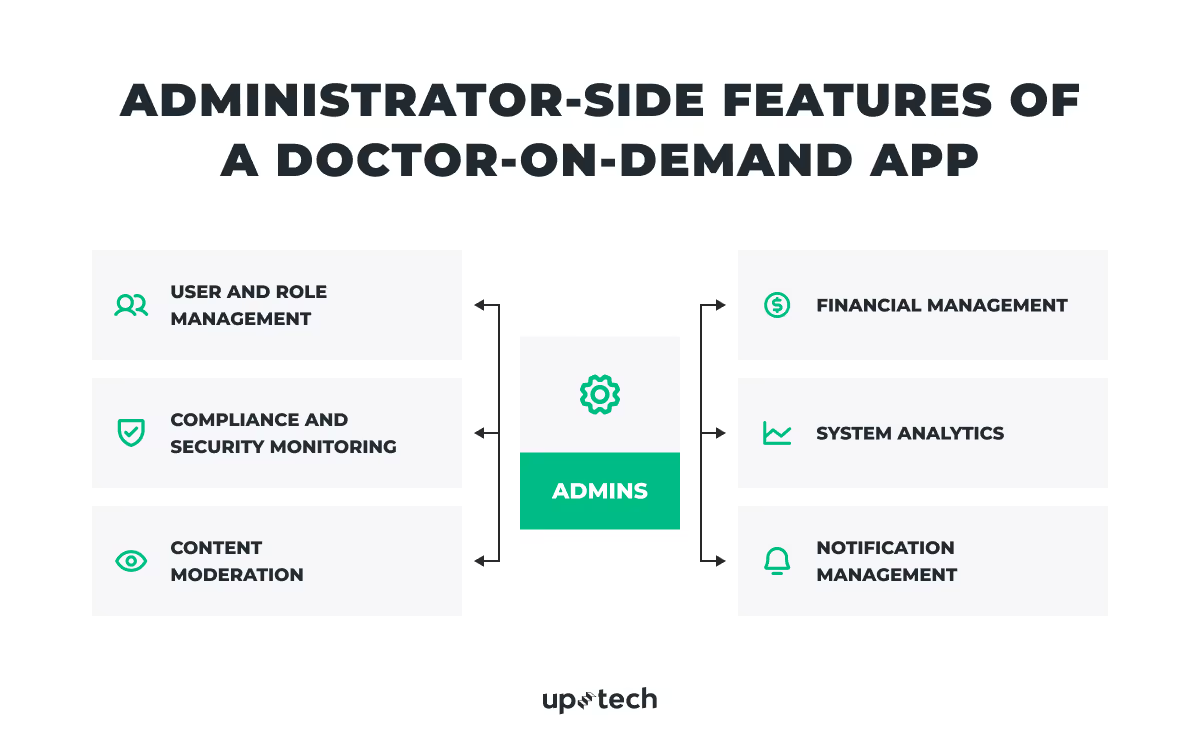
User and role management
Admins can create, verify, or suspend user accounts across both patient and doctor roles. Role-based access control (RBAC) separates data access levels and helps protect sensitive information.
Compliance and security monitoring
Auditing tools continuously track compliance with HIPAA, GDPR, and regional health data laws. Activity logs record every administrative action to ensure full traceability.
Content moderation
Built-in tools allow admins to review feedback, handle user disputes, and maintain a professional communication environment.
Financial management
Centralized dashboards provide clear visibility into transactions, commissions, refunds, and doctor payouts, ensuring accurate and transparent accounting.
System analytics
Reports on user activity, consultation numbers, conversion rates, and retention trends give admins insights for better operational and business decisions.
Notification management
Admins can configure push notifications, emails, and reminders to keep communication consistent across the platform.
UX/UI essentials for a doctor on-demand app
In telehealth, interface design directly affects clinical quality, patient safety, and trust.
According to the American Telemedicine Association’s Practice Guidelines for Direct-to-Patient Telehealth Services, usability and reliability are core determinants of patient engagement and clinical effectiveness. A well-designed interface is therefore not just aesthetic, but it is part of the standard of care.
Clarity, simplicity, and accessibility
Interfaces must communicate information in plain, unambiguous language and accommodate users with varying digital literacy levels. The AMA emphasizes that booking, consent, and payment actions should be completed within one or two intuitive steps. Interfaces should replicate the familiar rhythm of in-person care: registration, waiting room, consultation, summary, without unnecessary screens or data entry. Also, plain-language labeling to reduce cognitive friction.
For USA-based digital platforms, accessibility features, such as high-contrast modes, large typography, and screen-reader compatibility, are essential to meet both ADA and CMS telehealth access expectations, particularly for older adults and patients with disabilities.
Empathy and psychological comfort
Visual tone matters in telemedicine. Guidelines from the CDC recommend color palettes, typography, and imagery that convey calmness and professionalism, rather than a corporate detachment. Human-centered design with warm visuals, clear cues, and inclusive imagery helps reduce anxiety and builds an emotional bridge between patient and provider, which the AMA identifies as a determinant of perceived care quality.
Transparency and informed consent
Trust also depends on transparency about identity, pricing, and data use. Telehealth standards require a clear presentation of the physician's credentials, the telehealth service scope, and patient rights before the consultation begins. Data-handling notices, privacy statements, and secure-connection indicators should be visible and readable.
When these elements are embedded directly in the interface, they support compliance with HIPAA, GDPR, and state-specific consent regulations.
Doctor on Demand App Development Process
Once the core features are defined, the next step is to understand how to actually build a doctor-on-demand app. Below is a six-phase development roadmap you can follow. Of course, you can adapt this structure for your specific business needs and product vision.
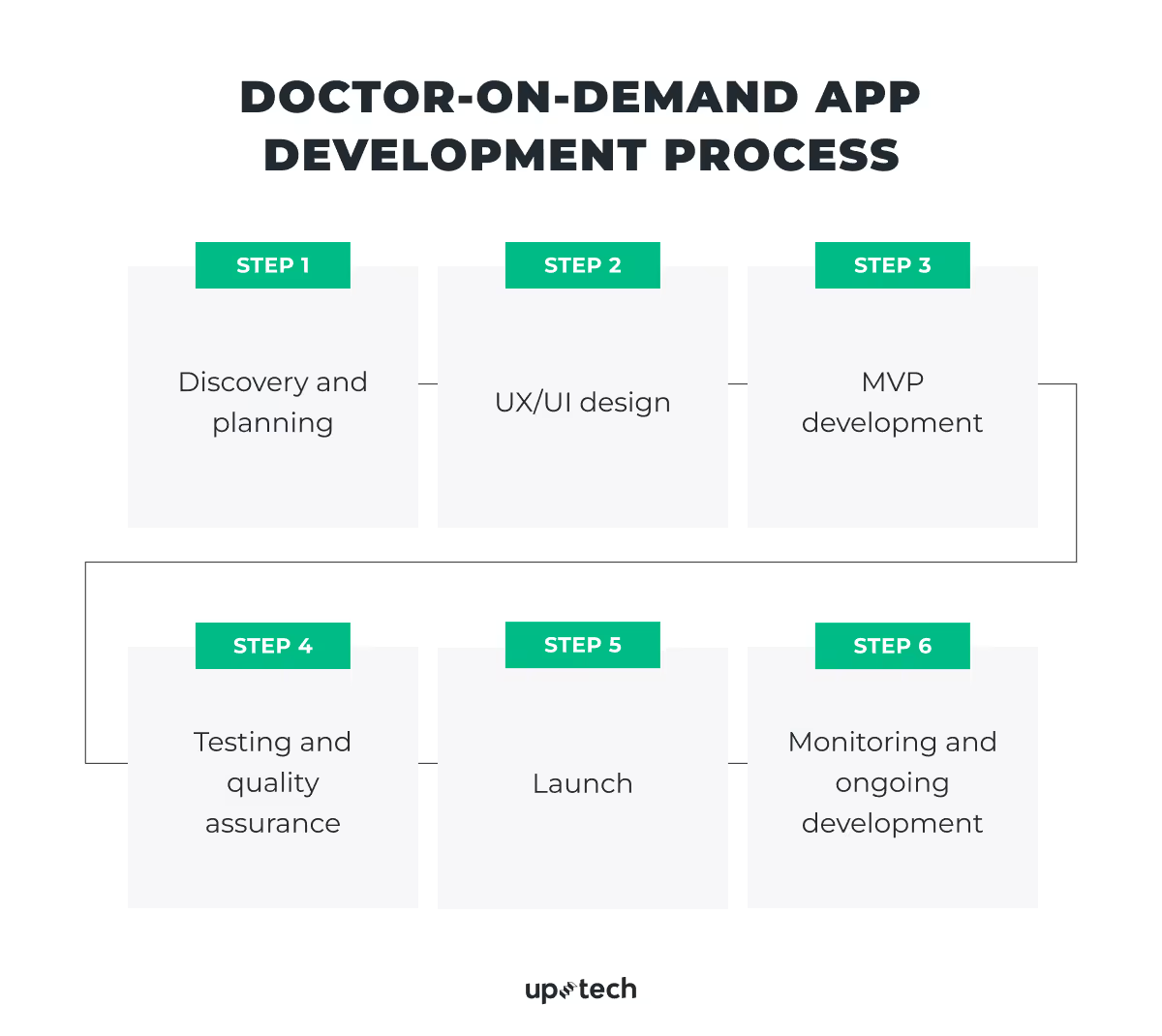
Discovery and planning
The goal of this stage is to align stakeholders, validate the product vision, and ensure regulatory readiness before any code is written.
What should be done during this stage?
- Stakeholder workshops and workflow mapping. Bring together clinical leaders and patients to map the current consultation process (registration → triage → consultation → prescription → follow-up). Identify inefficiencies and define how digital workflows can reduce friction.
- User and provider research. Conduct interviews with patients (trust factors, usage drivers) and doctors (scheduling pain points, workload, communication needs). Analyze accessibility needs, device constraints, and expectations for response time, privacy, and clinical accuracy.
- Regulatory and market assessment. Review HIPAA, GDPR, and FDA telehealth guidance. In the USA, check CMS telehealth coverage and reimbursement rules; in the EU, review cross-border data requirements.
- Business model and success metrics. Define measurable outcomes (patient retention, consultation length, revenue per provider, platform uptime). Choose a monetization model: per-session fees, subscriptions, or corporate wellness contracts.
- Product strategy and MVP scope. Prioritize must-have functionality: onboarding, doctor matching, video calls, prescriptions, payments, and chat. Defer complex features (AI triage, wearable integration) to later phases.
- Technical blueprint. With your engineering team or a Doctor-on-Demand development partner, outline a high-level architecture: backend, hosting, SDKs, and EHR integrations.
- Platform strategy. Decide where the app will run — iOS, Android, web, or a combination. Most providers choose both mobile platforms, but must also determine whether to build native or cross-platform apps, based on budget, performance needs, and audience behavior.
Key deliverables
- Product vision + OKRs
- User personas (patients, providers, admins)
- Regulatory and risk register
- Technical architecture diagram
- MVP scope, roadmap, and cost estimate
- Low-fidelity prototype of the main patient-doctor flow
UX/UI design
The aim here is to create trust-centric, accessible interfaces that simplify medical interactions for both patients and clinicians.
Focus areas during this stage
- Information architecture. Define modules for the patient app, doctor dashboard, and admin portal. Map data visibility.
- Core user journeys. Design every critical flow: registration, consultation booking, pre-visit questionnaire, live video session, payment, and post-visit summary.
- Trust and compliance cues. Following the ATA and AMA telehealth design standards, display verified doctor credentials, encrypted-connection icons, and visible consent language. Add a subtle reassurance copy, such as “All your data is protected.”
- Design system and consistency. Establish a reusable design system (color tokens, typography, button states, form rules) to keep accessibility and compliance uniform. Adhere to WCAG 2.1 guidelines for contrast and screen-reader compatibility.
- Prototyping and usability testing. Test interactive prototypes with real patients and clinicians. Measure time-to-complete, comprehension, and perceived care quality. Iterate quickly based on feedback to remove friction and strengthen trust.
Key deliverables
- End-to-end user flows and wireframes
- High-fidelity UI and component library
- Interactive prototype validated by users
- Accessibility and microcopy style guide
MVP development
The goal is to release a fully functional but focused version of the platform that validates business and clinical assumptions in real use.
Core functionality for this stage
- Patients: register, search doctors, book video consultations, make payments, and access summaries/prescriptions.
- Doctors: manage schedules, accept/reject appointments, host video calls, issue e-prescriptions, and review patient notes.
- Admins: oversee users, monitor system health, manage payouts, and view analytics.
Technical and security considerations
- Implement role-based access control (RBAC) and encryption.
- Store PHI data separately with strict access controls.
- Set up audit logging, MFA, and secure session handling from day one.
- Configure all cloud resources and any third-party providers (video calls, payments, analytics, etc.) to run under signed BAAs (U.S.) or DPAs (EU).
- Ensure data segregation between test and production.
- Integrate with EHR/EMR via FHIR APIs for continuity of care.
Timeline
MVP development typically spans 10–16 weeks, divided into 2-week sprints:
- Sprint 1–2: Authentication, scheduling, and user profiles.
- Sprint 3–5: Payments, prescriptions, video calls.
- Sprint 6: Admin panel, dashboards, compliance review.
Key deliverables
- Stable, secure MVP with core patient/doctor/admin functionality
- Compliance documentation (HIPAA/GDPR checklist)
- Deployment in a HIPAA-eligible environment
- Pilot feedback summary and iteration plan

Testing and quality assurance
Testing ensures that every feature works correctly, securely, and ethically, not just technically. Following telehealth guidelines, QA must validate both functional reliability and clinical usability.
Testing areas
- Functional: Ensure every patient–doctor flow works reliably — booking logic, notifications, payments, video sessions, prescription requests, and profile updates. Catching errors early is crucial because these flows directly affect care delivery.
- Performance: Stress-test the system to confirm it can handle peak-hour traffic, high concurrent video calls, slow networks, and mobile device limitations. Performance failures directly impact clinical reliability and patient trust.
- Security: Test for vulnerabilities — penetration tests, dependency audits, token validation, and encryption checks — to protect PHI. A single flaw can lead to compliance violations and reputational damage.
- Compliance: Validate consent flows, audit logs, retention rules, data-access rights, export/delete mechanisms, and documentation trails. Compliance gaps can block certification and limit platform launch in certain regions.
- Accessibility: Check screen-reader behavior, color contrast, navigation, and voice/keyboard support. Accessibility ensures legal compliance and unlocks usage across age groups, disabilities, and low-tech audiences.
- Interoperability: Validate FHIR/HL7 message exchange, lab integrations, and continuity-of-care records. Reliable interoperability prevents clinical errors and reduces admin workload.
Key deliverables
- QA test plans and coverage reports
- Penetration-testing and remediation logs
- Accessibility compliance statement (WCAG/ADA)
- Verified HIPAA/GDPR compliance report
Launch
The objective here is to deploy the app safely, provide operational readiness, and confirm that legal and support structures are in place.
Before launch:
- Upload assets, privacy labels, and documentation required by Apple/Google.
- Finalize Terms of Use, Privacy Policy, and signed BAAs/DPAs.
- Import verified provider profiles, specialties, and clinical documentation if migrating from an existing system.
- Train doctors and support staff on platform usage, escalation procedures, and privacy policies.
Pro tip: Start with a limited pilot to measure performance and user satisfaction before nationwide release. Monitor KPIs such as connection success rate, average consultation time, and patient CSAT. Gradually expand availability, adding advanced features via feature flags.
Key deliverables:
- Successful pilot launch with validated metrics
- Verified app store listings and compliance documentation
- Staff training materials
- Live monitoring dashboards and an incident-response plan
Monitoring and ongoing development
After launch, the focus shifts from building to maintaining reliability, security, and care quality.
Metrics to track:
- User and engagement: active users, repeat consultations, drop-off rate, satisfaction scores (CSAT/NPS).
- Technical health: uptime, API latency, video success rate, and crash-free sessions.
- Security: failed login attempts, unusual data exports, and admin activity logs.
- Business: average revenue per consultation, provider activation rate, marketplace fill rate.
Continuous improvement practices:
- Analyze user data to refine flows and reduce no-shows.
- Run quarterly security audits, SDK updates, and compliance re-validations.
- Conduct roadmap reviews with medical and compliance teams to ensure new features meet clinical and regulatory standards.
- Gather patient and provider feedback to guide ethical, human-centered growth.
Key deliverables:
- Centralized monitoring and alerting dashboards
- Quarterly performance and compliance reports
- Updated security and reliability documentation
- Roadmap of improvements validated by clinical and compliance leads
Common Challenges in Doctor-on-Demand App Development and How to Solve Them
Even the most carefully planned telehealth products encounter friction points once they move from concept to implementation. Doctor-on-demand–style apps are complex systems operating at the intersection of medicine, technology, and law, and each of these dimensions introduces its own risks.
Below are four recurring challenges that healthcare organizations, startups, and software partners face most often, along with evidence-based ways to resolve them.

Balancing compliance and innovation
Telehealth apps must remain agile to compete, yet every innovation is constrained by privacy and medical data laws, such as HIPAA, HITECH, and GDPR. Adding AI triage modules, integrating wearables, or automating prescriptions can unintentionally trigger new compliance obligations (for example, becoming a regulated medical device or processor of sensitive biometric data).
How to solve it:
- Embed compliance from day one: Define the applicable frameworks during discovery, not post-launch. Build “privacy by design” into architecture and UX.
- Appoint a data-protection officer (DPO) or HIPAA privacy lead: Their role is to maintain audit trails, consent logs, and access reports.
- Document every integration: Each third-party vendor (cloud, video SDK, analytics) must sign a Business Associate Agreement (BAA) or Data Processing Agreement (DPA), depending on the region.
- Use compliant clouds: HIPAA-eligible services from AWS, Azure, or Google Cloud allow PHI storage under a signed BAA (HHS Cloud Computing Guidance).
- Conduct regular risk assessments: Follow the HHS Security Rule checklist to test encryption, backups, and user access.

Managing doctor onboarding and quality
Scaling supply on the provider side is often harder than building patient demand. Telehealth success depends on a consistent pool of licensed, reliable clinicians. Without structured vetting and performance management, the quality of care, and therefore brand reputation, can drop quickly.
How to solve it:
- Apply credential verification: Automate license checks through APIs connected to national registries (like NPPES in the U.S. or GMC in the U.K.).
- Organize structured onboarding: Provide orientation on the app’s workflow, telehealth etiquette, and data privacy expectations.
- Create performance dashboards: Use anonymized post-consultation ratings, duration metrics, and adherence to clinical protocols to track consistency.
- Conduct peer review and continuous training: Partner with medical boards or e-learning providers to deliver quarterly micro-training on bedside manner, remote diagnostics, and digital documentation.
- Add transparent incentives: Reward responsiveness, patient satisfaction, and compliance adherence to motivate long-term engagement.
A disciplined provider-management program helps ensure patients receive care that meets professional standards across all regions and specialties.
Guaranteeing reliable video and platform performance
Patients and clinicians expect seamless, high-definition video, but telehealth operates in unpredictable environments: low bandwidth, mobile networks, and diverse devices.
A single dropped call can erode patient trust faster than any privacy issue.
How to solve it:
- Use proven video solutions built for telehealth. Choose technology that already handles poor connections, varied devices, and different environments so both doctors and patients get a consistently smooth experience.
- Test the platform in real-life scenarios. Before launch, check how the app behaves with slow internet, older phones, or peak-hour loads. This helps prevent issues patients might face once the app goes live.
- Define what “reliable” means for your business. Set clear expectations for call success rates, responsiveness, and platform stability. These benchmarks will guide improvements and show whether the experience is meeting patient needs.
- Make sure the system can grow with your user base. If your platform expands to new regions or adds more users, the underlying infrastructure should support that growth without quality drops.
- Monitor performance continuously. Track call quality and user reports in real time. Early detection of issues allows the team to fix problems quickly — often before patients even notice them.
Earning patient trust through branding and transparency
In healthcare, brand trust is inseparable from perceived care quality. Patients must believe their data is safe, their doctor is qualified, and the service is legitimate, especially when care happens remotely.
How to solve it:
- Show credentials clearly. Display verified provider information (licenses, experience, specialties) before booking, following AMA and ATA guidance on disclosure.
- Communicate privacy visually. Add consent prompts, encryption icons, and microcopy explaining data protection (for example, “Your consultation is encrypted and not recorded without consent.”).
- Publish clear Terms of Use and Privacy Policy compliant with GDPR standards; link them directly in the app footer.
- Use consistent, compassionate branding. Maintain calm colors, plain language, and an empathetic tone in all communication.
- Encourage feedback loops. Integrate post-visit surveys and public reviews to demonstrate accountability and transparency.
When patients perceive authenticity, control, and respect for their privacy, adoption rates rise, turning first-time users into long-term advocates.
Uptech’s Experience in Healthcare App Development
At Uptech, we’ve spent years helping to turn ambitious ideas into trusted healthcare digital products. Our goal has always been the same — to make complex medical processes simple, secure, and human-centered.
Our experience has shown that success in this space depends on two key factors: deep empathy for end-users — patients, clinicians, administrators — and rigorous attention to compliance, performance, and scalability.
Over time, we’ve partnered with companies across multiple healthcare domains.
Medical document processing system
A private clinic in the U.S. approached us to streamline and automate its growing operational workflows. Our dedicated team of engineers developed a web-based, AI-powered document processing system tailored to the clinic’s needs.
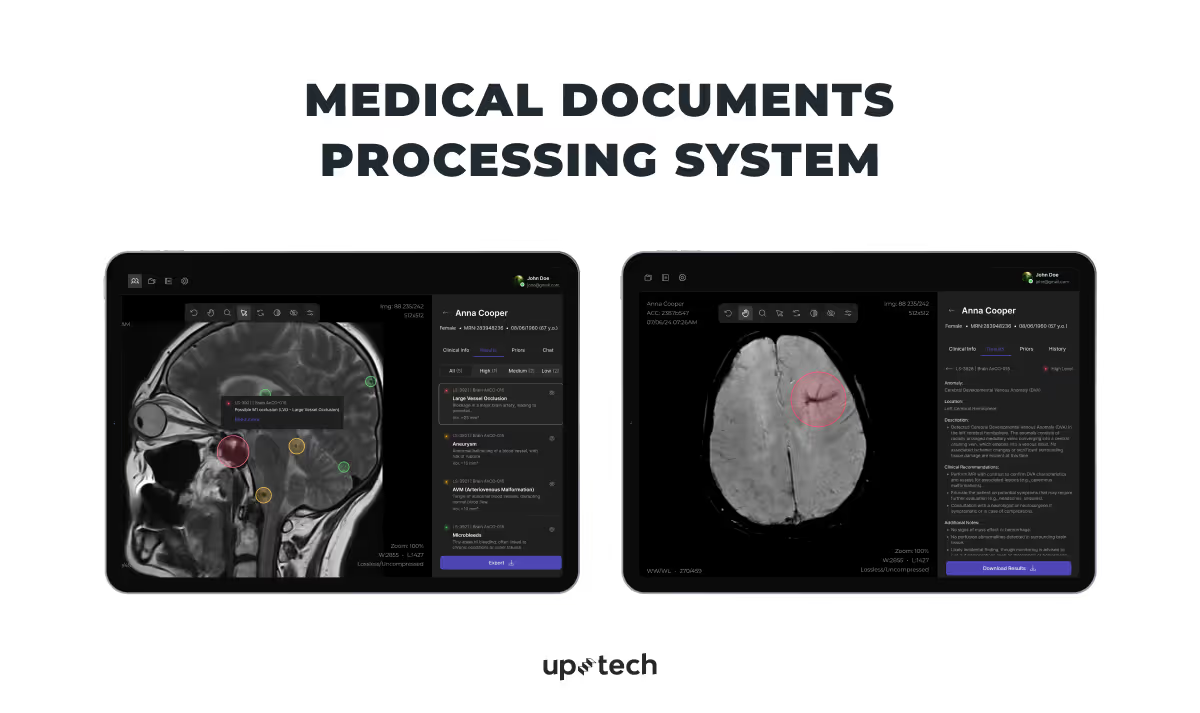
Our solution
We built a platform that uses OCR to digitize one-page typed documents and NLP to automatically classify them by type — including lab reports, prescriptions, and patient notes. An additional anomaly detection module flags potential issues such as missing data or conflicting test results, helping ensure record accuracy.
Results
After launch, the clinic reduced document analysis time by up to 30%, significantly improving workflow efficiency and allowing medical staff to focus more on patient care.
Check all the details in our full case study.
AI-powered prescription automation solution
Another one of our clients, a healthtech startup in Germany, turned to us to automate its prescription processing and reduce the heavy manual workload caused by diverse document formats. Our team of four engineers developed a web-based AI solution that streamlined the entire process — from data extraction to validation and output generation.
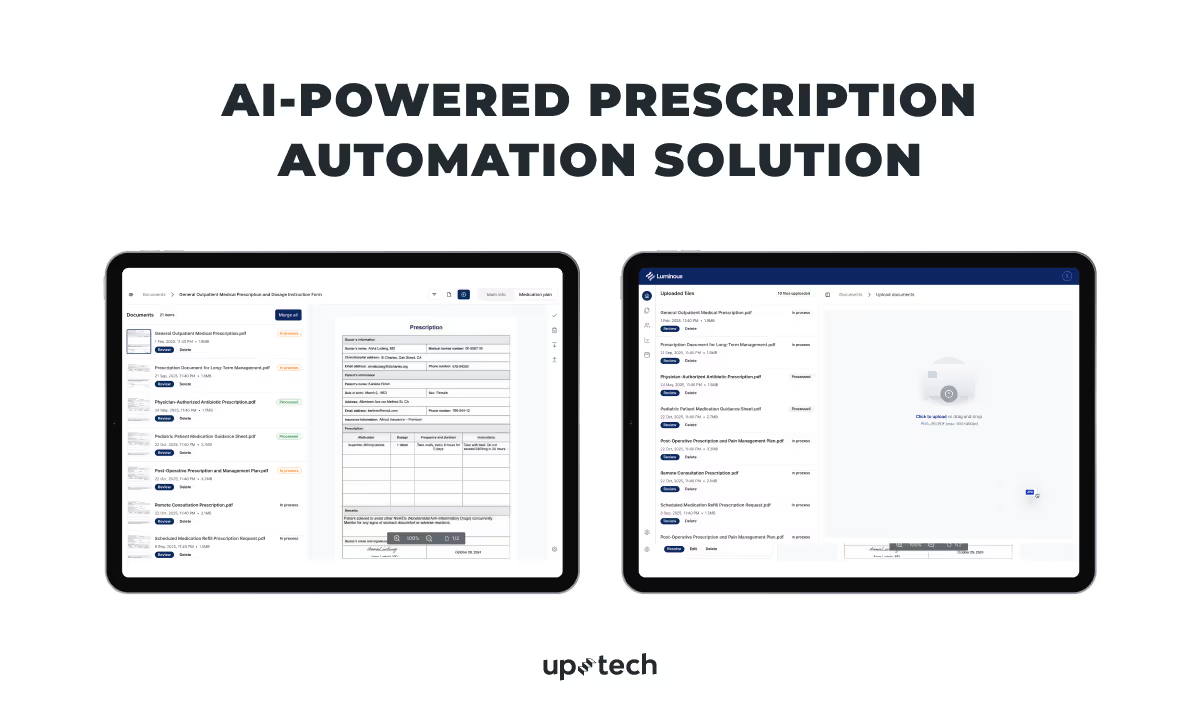
Our solution
We created a system powered by OCR and NLP that can read both handwritten and printed prescriptions, recognize key medical details, and convert them into structured digital data. The platform automatically merges multiple prescriptions into unified medication plans and generates barcodes for further processing. It also includes an error-detection module that flags incomplete or inconsistent data for review.
Results
The solution reached 85–90% accuracy in data extraction and classification. As a result, the client cut manual work, accelerated prescription handling, and built a more scalable foundation for their growing business. Check this case study to explore details.
Conclusion
Healthcare is moving toward a hybrid model in which digital and in-person care work together.
Virtual visits, AI tools, and self-service portals are no longer optional — they’re becoming the new standard. Doctor-on-demand apps play a key role in this shift by making care easier for patients and more efficient for providers.
The real value for healthcare organizations goes beyond video calls. A connected digital system that unites patient data, scheduling, payments, and clinical insights helps deliver care that’s faster, smarter, and more personal. Each interaction adds useful data that allows providers predict demand, improve engagement, and get better results.
At Uptech, we see healthcare technology not as a replacement for doctors, but as a way to amplify their impact. When empathy, compliance, and thoughtful design come together, digital health products can make care more accessible, trustworthy, and human.
Looking to build your own doctor-on-demand app? Let’s turn your healthcare vision into a secure, scalable, and patient-loved product that defines the next generation of digital care. Contact us for a free consultation.