Medical coding and billing are stressful and tedious. But they’re also instrumental in ensuring positive revenue growth for healthcare providers. Traditionally, medical billers and coders rely primarily on their judgment when scrutinizing thousands of codes. Their task got tougher, with ICD-11 taking effect in January 2022, prompting calls for AI medical billing solutions.
As healthcare providers transition to the new ICD standards, medical billers and coders must familiarize themselves with 70,000+ codes. Even if they could, coding mistakes are unavoidable, with past incidences causing taxpayers in the US $935 million weekly. Hence, AI is a timely intervention that healthcare providers badly need — to save them from more unnecessary losses.
I’m Dima Kovalenko, co-founder of Uptech. In this article, I’ll guide you through the opportunities of automating and streamlining medical coding with AI. After developing several AI-powered apps, such as Dyvo, Angler AI, and Hamlet, I’ll gladly help you navigate the complexities of building AI billing and medical coding systems.

What is Medical Billing?
Medical billing is a series of processes that document the medical services rendered to patients to ensure that healthcare providers are paid, either by the patient or insurance carriers.
Generally, a biller's job begins when patients register themselves and concludes when the billables are successfully collected. In between, medical billers went through several stages.

Collect patient information
Medical billers capture the required information when patients register themselves. They must fill in or update those details in the EHR system.
Doing so takes up substantial time, which calls for AI automation. AI technologies, specifically natural language processing (NLP) -powered apps, can speed up data entry.
Validate patient’s eligibility
Before proceeding with the procedures, billers must verify with the patient’s insurance providers that they’re eligible for claims. The process, however, can be time-consuming as both parties cross-check patient records. With AI, validation is automated, allowing billers to receive timely confirmations.
Prepare medical bills
As patients undergo treatment, billers prepare medical bills, which require consolidating patient records, diagnoses, lab results, and information from various EHR systems. Again, AI automation proves helpful. It automatically retrieves the necessary information, sparing billers from having to do them manually.
Submit claims to insurance carriers
Traditionally, billers send claims for approval manually and might need to call in to check on the progress. With AI, the process is automated, allowing billers to monitor the progress in real-time without any intervention.
Handle claim denials and appeals
Responding to claim denials can take up substantial time. Medical billers would have to revisit the rejected claims and identify errors or reasons for denials. Then, they would have to amend and resubmit the claim, consuming more time than they could spare. AI is capable of detecting patterns and preventing erroneous claims from being submitted. You can also train AI to recommend remediation actions to improve claim approval rates.
Process payments received
Once the claims are cleared, billers process checks or other forms of payments received. While most healthcare providers have software to handle this, AI allows them to forecast revenue growth and make necessary plans with predictive analytics.
Uptech – is an AI development company. Be on top of the new technology wave with our AI development services!
What is Medical Coding?
Medical coding is a discipline for transcribing a patient's diagnosis, symptoms, treatment, and other medical services they received into CPT, ICD, HCPS, or other medical codes. As part of the billing process, medical coding ensures that the payers are charged with the correct billables.
While medical coders don’t engage directly with patients or payers, their job is no less important. Generally, here’s what they do.

Assign medical codes to patient charts
Medical coders must decide the appropriate code that best describes the services, treatment, diagnosis, or prescription for every patient treated. Doing so is challenging because of the growing list of medical codes.
The IDC-10M alone contains 69,000 codes, and in the US, medical coders must juggle between 6 different HIPAA-mandated codes. Obviously, they would benefit from AI in medical coding. By using an AI assistant, they can quickly identify the correct code from a lengthy list.
Remediate claim denials
Like billers, medical coders play key roles in ensuring claims are approved. And when claims were denied, they would need to check for coding mistakes that escaped verification. Again, the process is painstakingly slow when performed manually. With AI, medical coders can speed up inspection, allowing a smoother and quicker resubmission.
Learn more about generative AI and how you can integrate state-of-the-art technology into your digital products.
How Specifically Can We Apply AI in Medical Billing?
AI brings vast opportunities to revolutionize medical billing to accelerate billing cycles and avoid costly errors. These are some prominent areas where AI can play a pivotal role.
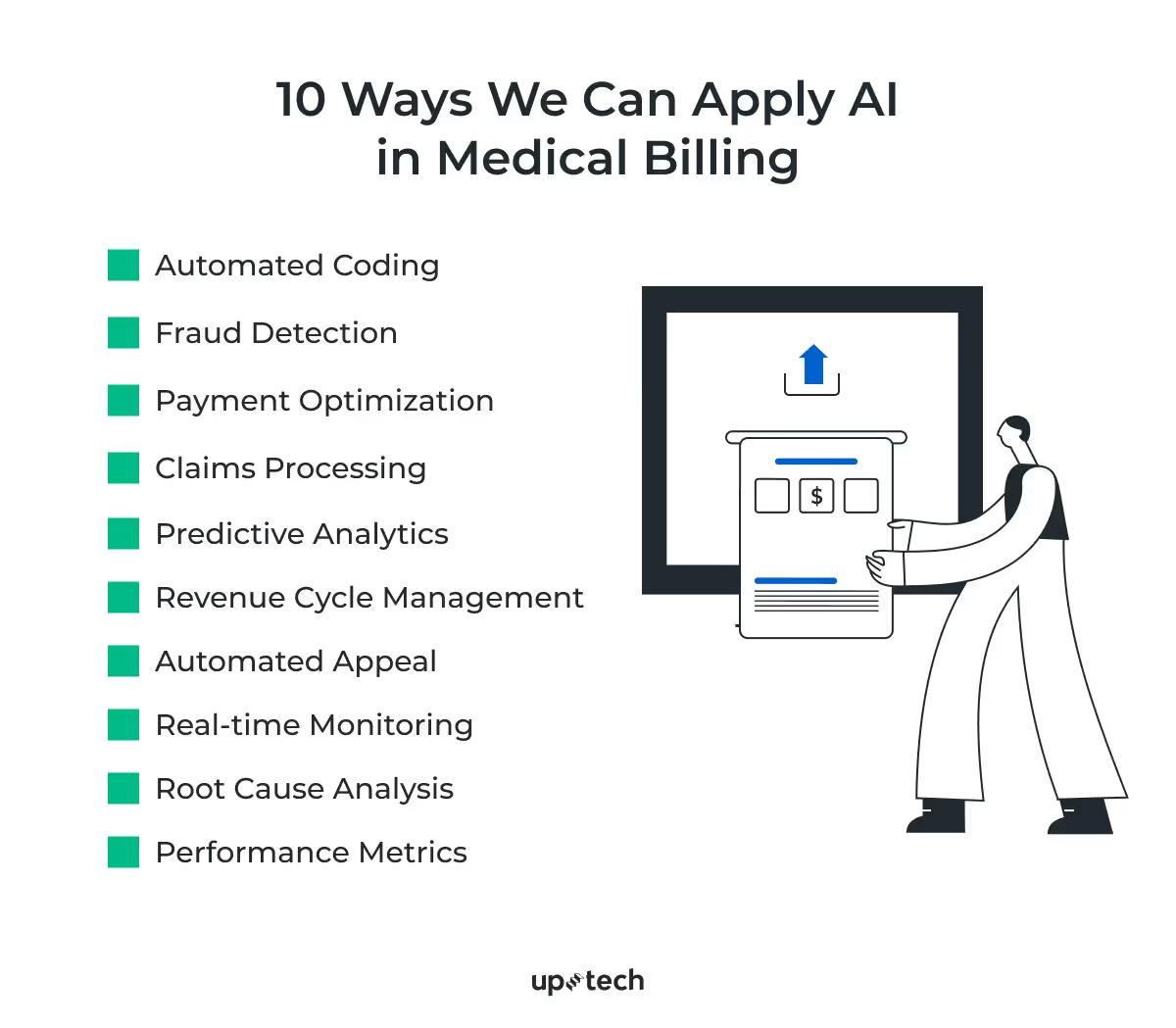
Automated Coding
As mentioned, medical coding requires broad medical knowledge to pick the correct code from thousands in the list. With AI, medical coders can confidently retrieve the appropriate codes without going through all of them. This way, healthcare providers can avoid coding mistakes and improve coding efficiency.
Fraud Detection
Another way AI can improve the financial outcomes of healthcare institutions and insurers is by reducing fraudulent claims. You can use AI to analyze claim documents to identify fraud and prevent financial losses.
Payment Optimization
AI has exceptional capabilities to predict future events based on past precedences. When integrated with financial systems, the technology helps predict payment patterns and allows healthcare providers to manage cash flow better.
Claims Processing
AI can pick up minute details that human eyes might miss. This proves handy when ensuring claim details are accurate before submitting them to the payers. Expect lesser rejection and a smoother reimbursement workflow with AI in medical billing.
Revenue Cycle Management
Your entire revenue collection workflow will benefit with AI in place. The technology can streamline and automate patient processes from end to end. Medical billing AI captures relevant data at all patient touchpoints to reduce billing errors, including registration, labs, treatment, and prescription.
Predictive Analytics
Instead of risking claim rejections, you can use AI to predict if medical claims will likely be approved. AI can detect coding errors, information mismatches, or other discrepancies that could jeopardize approval.
Automated Appeal
Even if your claims are rejected, AI can automatically resend them for appeal after correcting all the mistakes. This helps billers skip the additional resubmission steps that they do manually.
Real-time Monitoring
With AI, you can effortlessly track the claims you submitted. Billers will receive timely alerts on potential issues and remediate them to ensure they’re successfully processed.
Root Cause Analysis
Procedural flaws, human oversights, and other factors may result in abnormally high rejections when you submit claims. Medical billing AI software can analyze and find distinct patterns from multiple claims to reveal possible rejection factors.
Performance Metrics
AI can also monitor the entire claim reimbursement pipeline to identify areas of strengths and weaknesses. You can generate charts and reports to optimize the medical billing lifecycle.
We design and develop healthcare software for doctors, hospitals, labs, medical manufacturing companies, and healthcare startups. Our clients say that we work fast, come up with innovative ideas, and build great and quality apps. Check what custom healthcare software development services we offer.
Types of Artificial Intelligence in Medical Billing
Artificial intelligence is a broad term that includes several evolving technologies that will impact conventional medical billing workflows. I share several types you ought to pay attention to below.
Machine learning
Machine learning (ML) is an approach that trains software to make decisions like humans with data. To develop ML medical applications, you need to engage data scientists, machine learning engineers, and software developers. They would then create the ML algorithms, curate the required datasets, train the model, and fine-tune it to enable practical usage.
For example, you can train medical coding software to associate ICD codes with respective symptoms with curated copies of medical notes. Then, the ML-powered software can automatically detect and assign ICD codes to patient charts.
Learn how to train, develop, and deploy an AI diagnostic tool for healthcare professionals.
Natural language processing
Natural language processing (NLP) is a subdiscipline of machine learning that enables computer systems to understand and respond in conversational languages as humans do. In medical billing, you can apply NLP to various applications, including transcribing patient conversations, detecting medical terminologies, and processing patient records.
Like ML systems, developing NLP software for medical billing and coding requires a team of data scientists, machine learning engineers, and software developers.
Computer vision
Computer vision is a field in artificial intelligence that focuses on extracting, processing, and understanding geospatial features from visual data. Often, medical billers are overwhelmed with paperwork that computer vision software can help. For example, you can use computer vision to develop software that can understand scanned images, text, or reports and automatically record them into EHR systems.
Check what challenges clinical documentation systems face and how AI can offer transformational changes.
Engage computer vision engineers, machine learning teams, software developers, and data scientists if you need to build CV digital systems.

Why Does AI Matter to Your Billing, Coding, and Efficiency?
The problem with medical coding and billing is — it’s an error-prone process that’s extremely difficult to scale. Healthcare providers struggle to keep up with the growing medical codes. Training more medical coders is simply not an option. Besides, solely relying on human coders risks costly expenses, inefficiencies, and delayed payments. Likewise, following up with claims, crosschecking financial records, and submitting rejected claims are equally taxing.
With AI, medical billers and coders can reduce mistakes and avoid getting burnout on the job. Here’s how.
- AI chatbots with NLP capabilities can assist medical billers in interacting with patients and filling out registration records.
- Billers can improve patient engagement by analyzing their behaviors with AI and following up with personalized responses.
- Instead of anxiously inspecting for errors, billers and coders can leverage AI to alert them of missing, incorrect, or abnormal data in medical records.
- Whether transcribing speech or analyzing lab imaging results, medical teams benefit from speech recognition, language processing, and computer vision capabilities that AI offers.
- Predictive intelligence allows billers and coders to anticipate and fix problems, particularly when preparing claims.
- Medical billing automation brings disparate processes together in the healthcare revenue lifecycle. Billers no longer need to manually call insurers to check for approvals or switch between different platforms to cross-check patient records.
Privacy and Other Concerns of AI in Medical Coding and Billing
Undoubtedly, AI has plenty to offer to medical coders and billers. Yet, adopting medical AI systems faces challenges and pushback from various stakeholders.
Privacy challenges
Training and operating AI medical systems require collecting, processing, and storing sensitive health data on software and cloud infrastructure. Patients are concerned that their health and financial information might be compromised and abused by bad actors. Without adequate protection, such as encryption, data breaches might occur.
Implementing medical billing and coding solutions requires strict compliance with data privacy regulations, whether with AI or not. For example, your app must comply with:
- Health Insurance Portability and Accountability Act (HIPAA), which regulates how US healthcare providers manage patients' data and safeguard their privacy.
- General Data Protection Regulation (GDPR), an act requiring healthcare providers operating in the EU region to obtain consent from patients before they can store or process their data.
- Personal Health Information Protection Act (PHIPA), a data privacy act that Canadian medical providers must comply with when managing protected health information.
It’s important to understand that developing and implementing medical coding and billing systems is layered with complexities. Moreover, not all app developers are knowledgeable or experienced in HIPAA. Hence, it’s better to collaborate with a HIPAA-compliant certified partner to avoid violating regulations.
Uptech, for example, has a commendable record of developing HIPAA-compliance apps for the US healthcare market. Our team employs stringent security measures to safeguard patients' data from all interaction points. More importantly, we understand the complexities of bringing together AI, cloud, and other tech stack to produce safe, intuitive, and functional medical apps.
If you’re keen on leveraging the opportunities that AI brings, read on and learn how to establish an AI governance framework to support your healthcare product.
Skilled medical coders
The challenge that healthcare providers face is the lack of skilled medical coders. AI systems are helpers, not replacements for human medical coders. Despite AI’s promises, healthcare providers still need to secure the services of skilled medical coders. AI, as helpful as it is, requires safeguards to ensure they perform as intended. Furthermore, medical coders play a vital role in fine-tuning an AI model because it can automatically assign ICD codes.
Data scarcity
Training AI systems to automate medical billing and coding requires curating and annotating large volumes of healthcare records. Unfortunately, obtaining the records necessary to train and fine-tune a model is challenging. Without adequate training, AI systems will not perform well in the real world. Hence, AI developers use techniques like data augmentation to compensate for the lack of training data. Data augmentation is a method that ML engineers use to increase the dataset size by creating modified copies from the original training data. It’s a popular approach to train AI models, particularly for healthcare applications.
Integration with other EHR systems
To fully automate and streamline your billing processes, you need to integrate medical AI software with existing or third-party software. Data incompatibility, protocol differences, and legacy software are obstacles to rolling out a fully automated AI medical and billing system.

The Future of Medical Coding and Billing
Medical coding and billing are vital in supporting the increasing demand for transparent and professional healthcare experience. Studies indicated that medical coding commands a sizable market value, growing at 9.35% CAGR from USD 18.2 billion in 2022. And that’s contrasted by the fact that 30% of claim denials that hospitals face stem from coding mistakes.
Key stakeholders are anticipating several developments that might resolve payment issues that troubled the healthcare industry.
- Emerging AI technologies, like generative AI and computer vision, will automate medical coding and billing, resulting in fewer coding errors.
- New regulations, such as the No Surprises Act, require healthcare providers to provide transparent and accurate bills for services patients receive.
- Patients expect exceptional care deliveries, which include hassle and mistake-free billing experience.
These expectations offer the opportunities to integrate AI with medical billing and coding that healthcare providers should capitalize on. As mentioned, AI holds transformational potential, but there are barriers to organizational-wide adoption. You’ll have a better chance of rolling out these changes by partnering with a HIPAA-compliant AI developer — particularly one experienced in healthcare apps.
Talk to our team today and start automating your medical billing and coding with AI.
FAQs
What is the role of AI in medical coding?
Medical coding requires human coders to look through tens of thousands of codes and select one that best describes treatment, services, symptoms, or other medical conditions. AI can automatically retrieve the code by analyzing medical records and patient data.
Can AI do billing?
AI can automate most parts of medical billing, such as verifying eligibility, registering patients to EHR systems, submitting claims, and managing denials. This frees billers from spending excessive time on repetitive and mundane tasks.
What is Gen AI in medical coding?
Gen AI, or generative AI, is artificial intelligence capable of producing unique content from the knowledge it learned from. In medical coding, generative AI can learn from medical codes like CPT, ICD, and HCPS and help coders fill the respective codes in patient charts.