Telehealth has firmly moved past its pandemic moment. Today’s telehealth trends reflect a shift toward permanence and more disciplined execution across healthcare delivery.
After years of fast growth followed by market correction, the focus has turned to making telehealth work well at scale. The conversation is now about how it fits into everyday care, how reliably it performs over time, and how it holds up as a long-term system.
You can already see this shift in how platforms are used, where capital is flowing, and how digital products are changing. Together, these signals show where telehealth is headed in 2026.
But before looking ahead, let’s step back and briefly revisit how telehealth grew into its current form and where the market stands today.
How Telehealth Became a Core Part of Healthcare
Telehealth was rolled out quickly and stayed.
Usage never dropped back to pre-COVID levels. After the initial surge, telehealth stabilized at roughly 38× the pre-pandemic level, indicating that virtual care addressed a lasting structural need rather than a short-term workaround.
Many startups that had been experimenting with virtual care suddenly found themselves at the center of mainstream healthcare delivery.
One clear example is Teladoc Health. In 2020, the platform handled 10.6 million visits, a 156% increase year over year. Revenue nearly doubled as well, reaching $1.094 billion, up 98% from the previous year.
Amwell saw a similar surge. In 2020, the company reported 65% revenue growth as demand for virtual care infrastructure spiked. Its active provider base expanded dramatically, growing from roughly 7,000 to 72,000 clinicians — an increase driven by fast, large-scale onboarding during the pandemic.
Tools that once played a secondary role in healthcare delivery suddenly became essential, accelerating long-term telemedicine trends. Telehealth moved from “nice to have” to core infrastructure almost overnight.
Investment followed demand. According to McKinsey, funding for digital health nearly doubled compared to 2019 levels.
Today, the picture looks different. The pandemic surge in virtual care trends is over, and venture capital has cooled compared to peak years. But money hasn’t disappeared. Investors are now focused less on growth at any cost and more on outcomes and sustainable performance. This shift has quietly reset trends in telehealth, pushing platforms to prove long-term clinical and operational value.
In 2025, the telemedicine sector raised $2.35 billion, marking a 10% increase year over year. The pace is slower than during the pandemic boom, but it signals that telehealth has moved into a more mature, disciplined phase of growth.

What This Sets Up for 2026
Digital health is still moving fast. AI adoption is accelerating, and telehealth remains one of the most active areas for real innovation in healthcare.
So what should we expect in 2026? Which telehealth trends will shape healthcare, and what will they mean for product teams, innovators, and business leaders?
Drawing on my product management background and experience in telemedicine app development solutions, here are a few practical observations and assumptions about future virtual healthcare trends.
Let’s get started.
Telehealth Trends Shaping Healthcare in 2026
Telehealth is now a permanent part of healthcare. Years of fast adoption, shifting regulations, and changing expectations from both patients and providers have shaped how it works today. Several clear trends in telemedicine are already visible across the market.
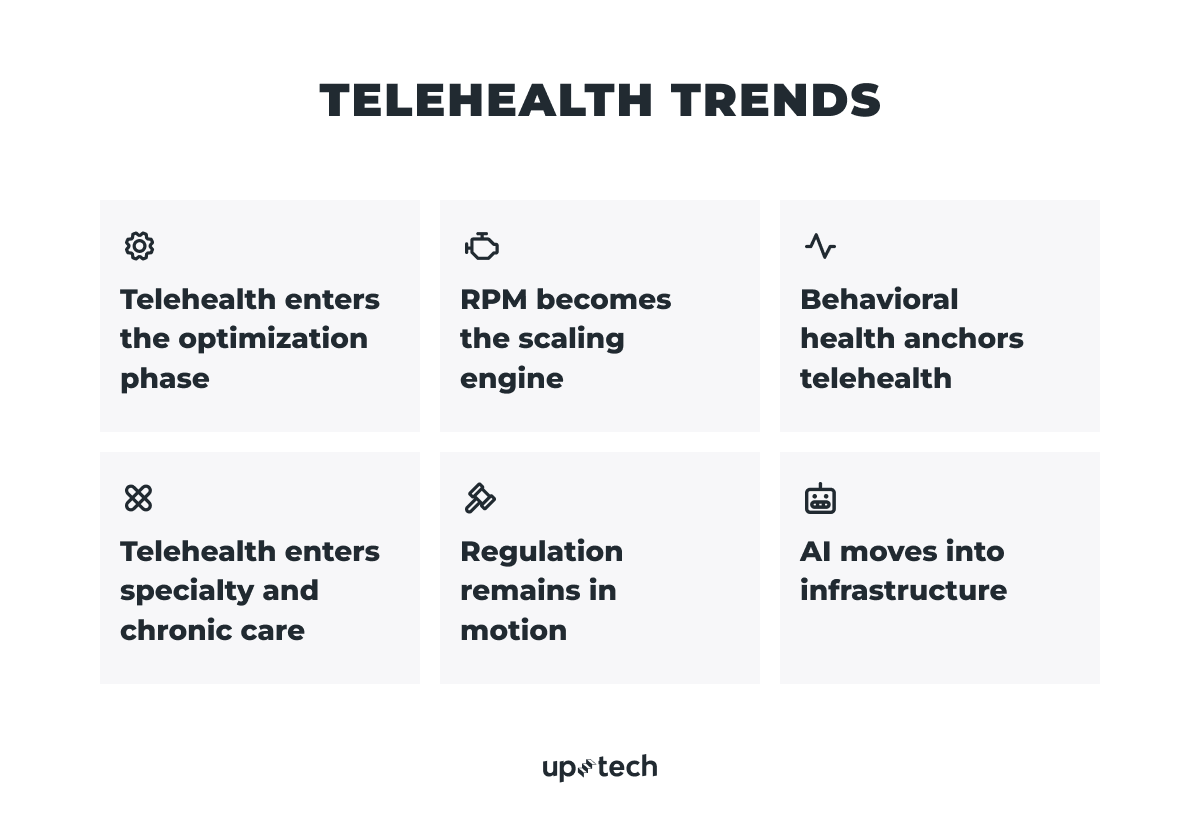
Telehealth shifts to optimization
In 2026, telehealth is neither booming nor fading away. It has become a stable part of care delivery. Over 71% of physicians globally, including in high- and middle-income countries, say they use telehealth tools weekly.
That stability changes what success looks like and reframes current telemedicine trends.
When telehealth was still new, the main question was volume:
How many virtual visits are happening? How fast is usage growing?
Today, those questions matter much less. Telehealth is expected, and the real difference between providers now is not whether they offer it, but how well they run it.
As telehealth matures, quality and operations become the main differentiators.
Two systems can have similar visit volumes and very different results. The gap shows up in:
- Conversion rates
- No-show rates
- Clinician productivity
- Total cost of care
Poorly designed workflows create friction. Patients drop off. Treatment is delayed. Costs rise. Well-designed workflows do the opposite: they shorten time to treatment, reduce unnecessary touchpoints, and resolve issues faster.

Because of this shift, performance metrics are changing.
Instead of tracking “telehealth adoption,” leading teams focus on:
- Leakage — where patients abandon the process
- Time to treatment, not just time to a scheduled visit
- Cost per resolved episode, not cost per encounter
The logic is simple: value comes from solving the problem, not from completing a call.
2025 clinical and implementation research highlights that success in telehealth depends on strong infrastructure, appropriate platforms, technical support, and digital literacy.
Growth brought telehealth into the system. Operational excellence will determine who actually benefits from it.

RPM becomes the scaling engine
For years, telehealth was almost synonymous with video visits. That made sense during COVID, when the main problem was access. Patients couldn’t get to clinics, and video calls were the fastest workaround.
By 2026, that logic no longer holds.
Video visits solved an access issue. They did not solve healthcare’s deeper problems: limited clinical capacity, growing chronic disease, clinician burnout, and the need for ongoing, not episodic, care. This is where remote patient monitoring (RPM) takes center stage.
Nearly 50 million Americans are already using some form of remote patient monitoring (RPM), and 8 out of 10 people say they are open to using RPM as part of their medical care. Clinicians are adopting it just as quickly. By 2023, 81% of providers reported using RPM, up more than 300% compared to 2021.
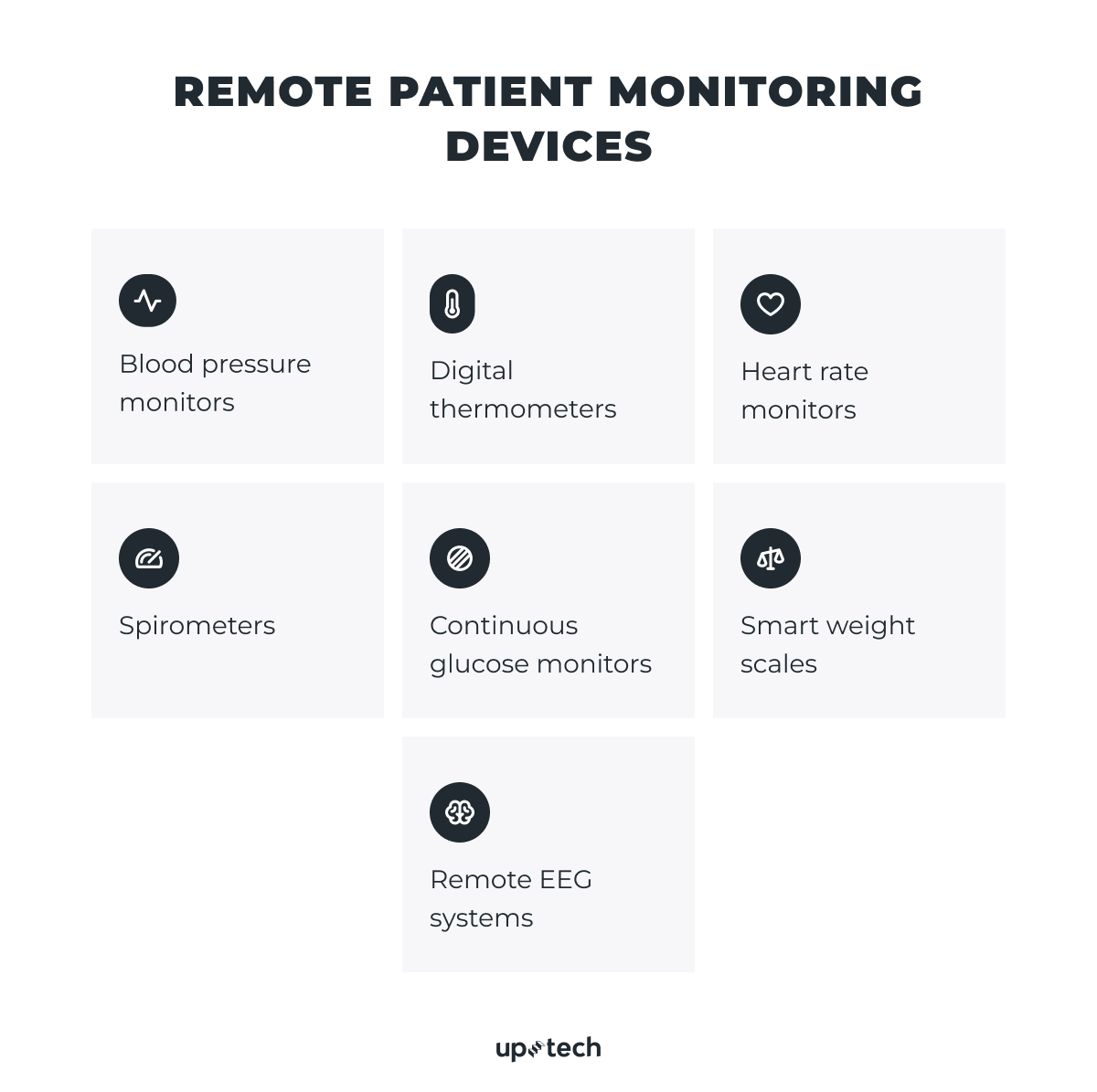
RPM shifts telehealth trends away from one-off appointments toward continuous, asynchronous care.
AI integration in RPM is growing rapidly, too: the AI-focused RPM market alone is projected to grow at a CAGR of ~27.5% through 2030, showing how analytics and predictive monitoring are becoming part of standard care delivery.
Instead of relying on scheduled conversations, care is driven by ongoing data, clear protocols, and targeted intervention. Clinicians don’t need to be present at a specific moment to deliver value. Data flows continuously. Human attention is used only when it’s clinically necessary.
That shift fundamentally changes how care scales and shapes many of today’s virtual healthcare trends.
What actually makes RPM work
RPM is more than a simple device strategy.
Many programs fail by treating it like a hardware rollout: ship devices, connect dashboards, and expect clinicians to “check the data.” That approach doesn’t scale.
Successful RPM programs operate like clinical operations systems. They clearly define:
- Who reviews incoming data, and how often
- What level of training is required at each step
- When and how escalation happens
- How reviews and interventions are documented
They rely on protocol-driven workflows and enforce documentation discipline, so every action is traceable, clinically meaningful, and billable. And they generate payer-grade reporting that proves utilization, responsiveness, and outcomes.
The benefits of RPM
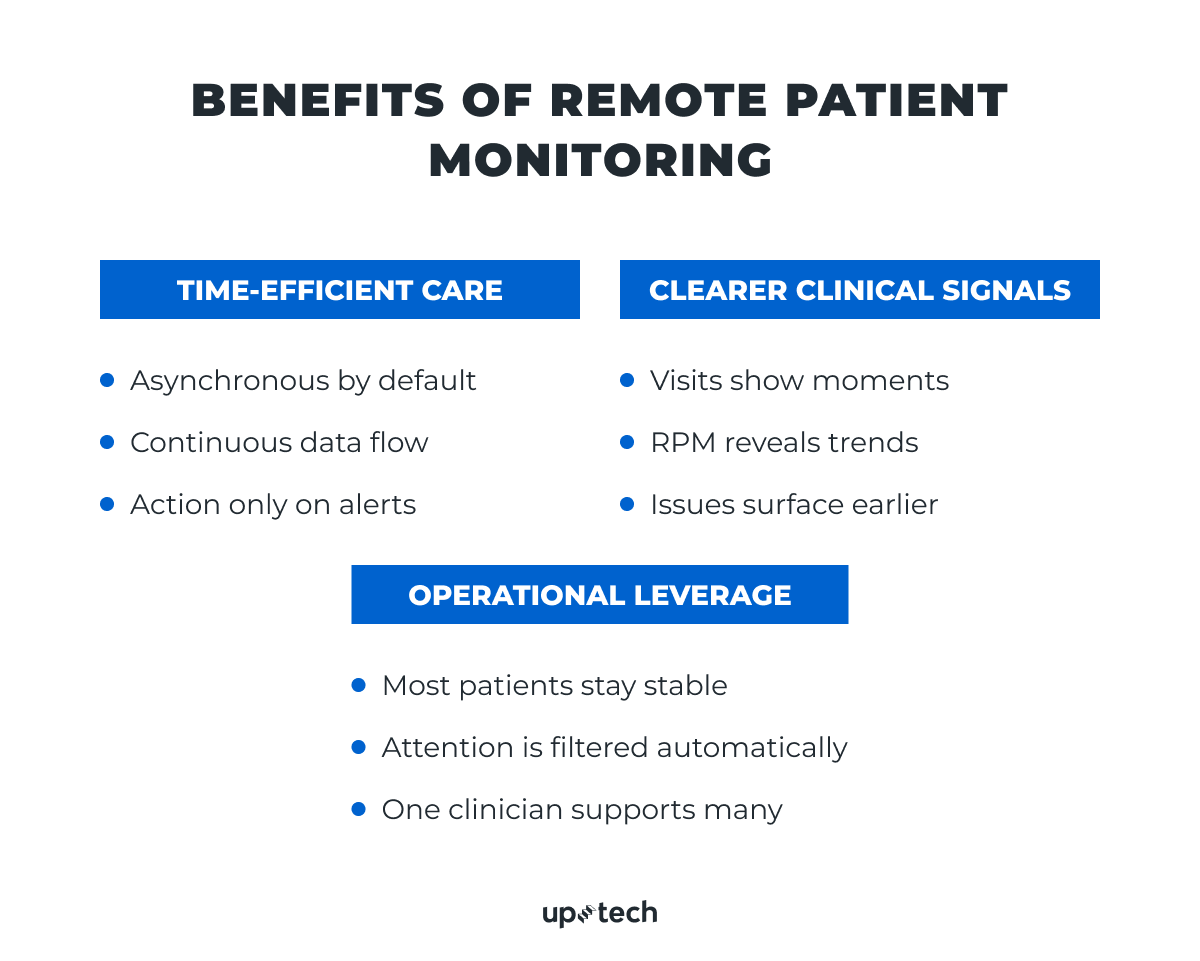
- RPM breaks the time lock. Video visits require the patient and clinician to be present at the same time. RPM does not. Vital signs, symptoms, and adherence data arrive continuously. Predefined clinical thresholds and alert rules flag deviations from a patient’s baseline, allowing clinicians to review information in batches or respond only when thresholds are crossed. Less waiting, less wasted time.
- RPM produces better clinical signals. A single visit captures a moment. Monitoring over days or weeks reveals trends: gradual decline, variability, missed medications, and early warning signs. Sometimes these patterns are far more useful than isolated data points from a short call.
- RPM creates operational leverage. Most patients are stable most of the time. With RPM, one clinician can safely oversee dozens of patients, stepping in only when escalation is needed.
Video visits still matter, but their role changes. They become escalation points, not the default mode of care. Continuous monitoring does the day-to-day work. Video is reserved for moments when human interaction is truly needed.
Behavioral health anchors telehealth
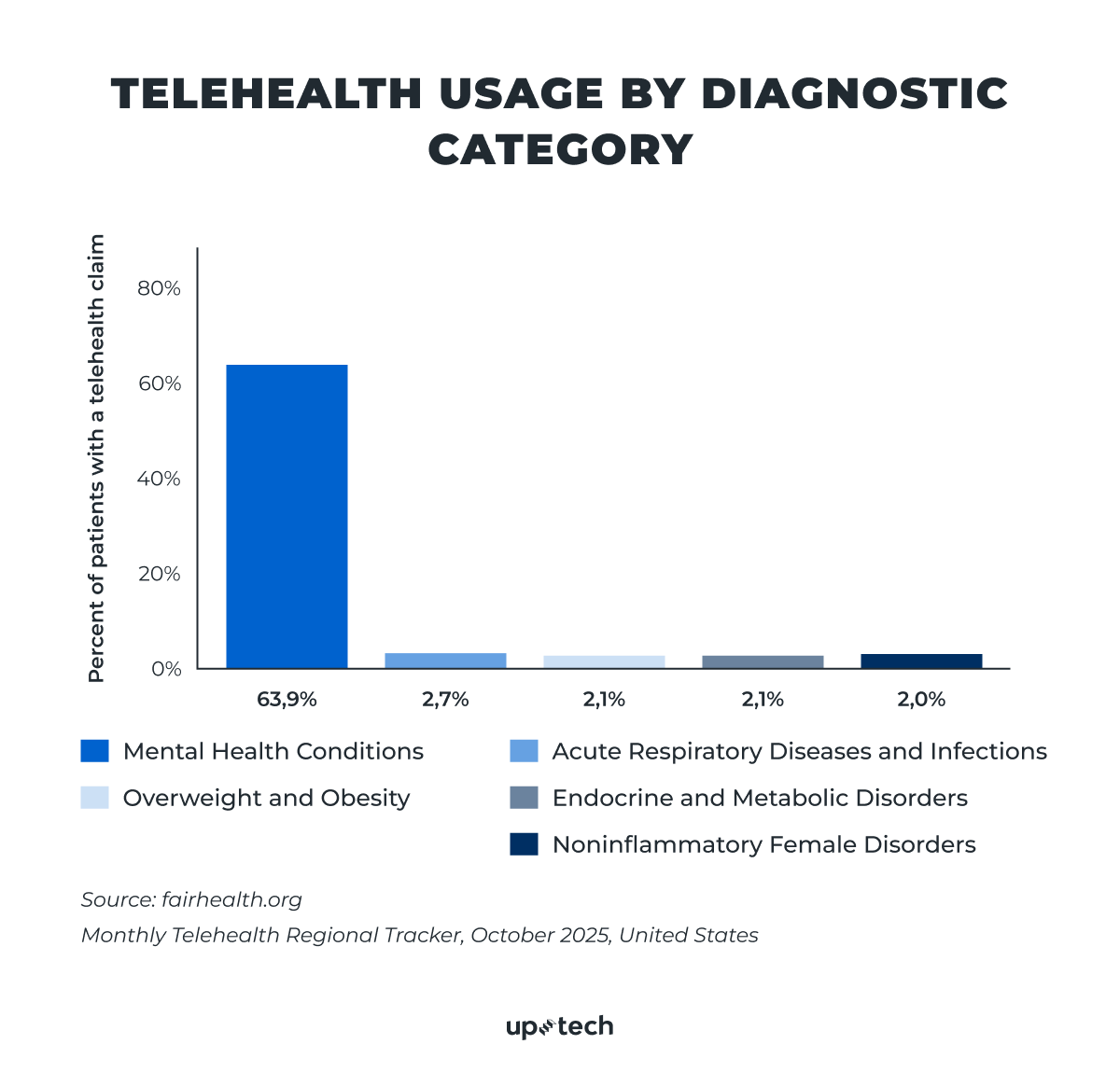
Across all telehealth categories, behavioral health stands out as the most stable and durable area within current trends in telemedicine. In early 2025, data showed that about 58–62% of telehealth claims were for mental health conditions — more than any other diagnostic group.
Demand remains high, usage is consistent, and care delivery depends far less on physical exams or in-person procedures than in most other specialties. Because of this, behavioral health has proven to be well-suited to remote care.
Why behavioral health works remotely
Mental health care is built on conversation, trust, and continuity. Visuals and physical interaction matter far less than they do in other areas of medicine. In many cases, the quality of care depends more on whether a patient can show up regularly than on whether the session happens over video.
A good example is Clearly, a mental health marketplace we worked on. The platform supports over 30,000 therapy sessions each month, and 98% of clients report positive changes after their first session.
Telehealth’s role in increasing access to behavioral care for people who might otherwise face barriers due to distance, transportation, or clinician shortages. For example, in the United States, more than half of the counties lack psychiatrists, underscoring why remote options remain critical.
That flexibility is a major reason behavioral health has remained resilient while other telehealth use cases have fluctuated.
The continued importance of audio-only care
Audio-only care still plays a critical role in maintaining access.
For many patients, video is not always realistic or comfortable. Limited broadband, shared devices, lack of private space, or anxiety about being on camera can all become barriers. Data on telehealth policy and past utilization show that older adults, in particular, used audio-only visits more often than video visits.
In these situations, audio-only sessions are not a lesser option — they are often the difference between staying in care and dropping out altogether.
From an accessibility perspective, audio-only is a great additional inclusion mechanism and remains relevant this year.
Policy is moving toward hybrid, not back to in-person
Moreover, behavioral health faces fewer geographic and modality restrictions than many other specialties, and audio-only care remains permitted under defined conditions.
Looking toward 2026, policy direction increasingly supports hybrid models. Periodic in-person visits are layered into long-term treatment relationships, while remote care remains the default. This does not weaken telehealth, but rather formalizes how it is already being used in practice.
In 2026, behavioral health will continue to anchor telehealth strategies — not because it is the most technologically advanced area, but because it aligns best with how remote care actually works.
Telehealth enters specialty and chronic care
Telehealth is no longer limited to quick consultations or urgent care. It is increasingly expanding into specialty medicine and long-term condition management.
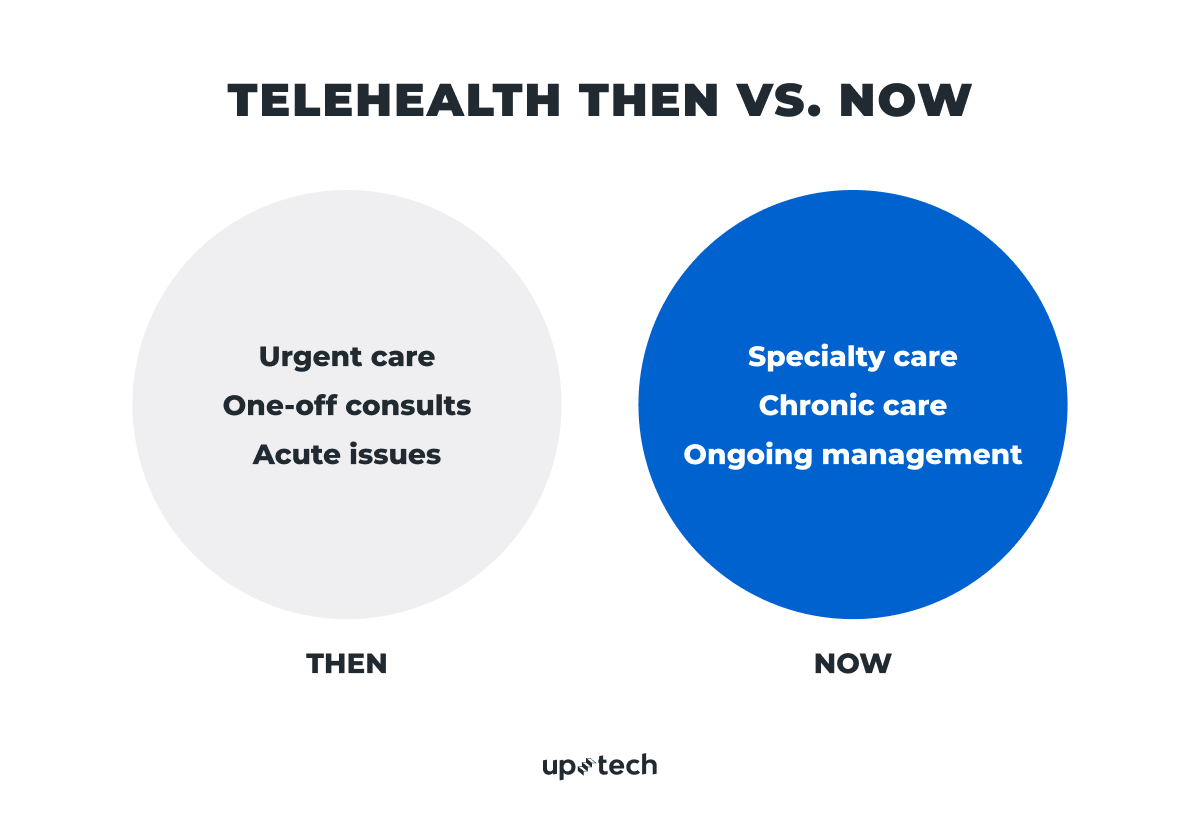
Most care delivery and spending are tied to chronic conditions, not acute episodes. Diabetes, cardiovascular disease, endocrine disorders, and many dermatological conditions require regular monitoring, behavioral support, and ongoing adjustment — not frequent in-person visits. Telehealth fits naturally into this pattern.
A recent survey from the American Medical Association (AMA) found that telehealth was used regularly for ongoing care in several specialties beyond psychiatry, including neurology (32% of visits), endocrinology (24%), and gastroenterology (20%).
Telehealth in chronic care management
In chronic care, telehealth enables a steady, ongoing connection between patients and care teams.
Remote check-ins, symptom tracking, and data review help surface issues earlier and keep patients engaged between formal appointments. Instead of care happening only during clinic visits, it becomes continuous and proactive.
This approach reduces gaps in care and lowers the risk of problems escalating unnoticed.
Telehealth’s growing role in specialty care
Many specialty follow-ups are data-driven rather than procedural.
In areas like preventive medicine, clinicians often need to review images, lab results, or patient-reported outcomes rather than perform physical interventions. Handling these interactions remotely reduces wait times, lowers travel burden for patients, and frees up in-person capacity for higher-complexity cases.
Telehealth as the digital front door
Telehealth is also becoming the entry point for primary care.
Instead of starting with phone calls and manual scheduling, patients move through structured online intake, triage, and routing. This improves access while reducing unnecessary appointments and administrative load on care teams.
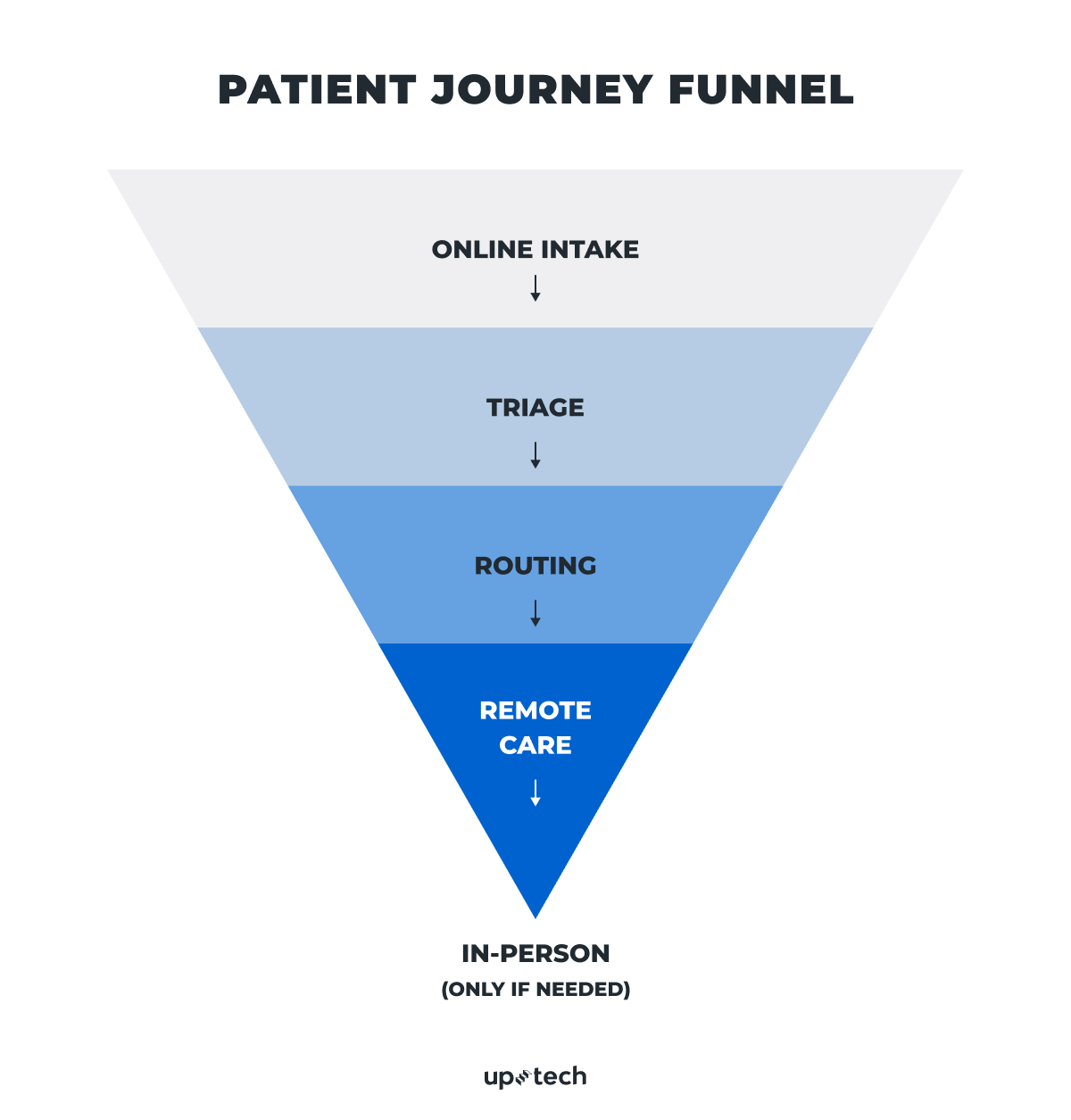
In-person care is reserved for moments where it adds the most clinical value.
As telehealth expands beyond urgent care, success depends less on convenience alone and more on how well it supports sustained, coordinated care over time.
Regulation remains in motion
Telehealth does not operate in a regulatory vacuum, and that won’t change in 2026.
Many of the flexibilities introduced during the pandemic are still in place, but they were never meant to be permanent. What we are seeing now is a transition: policy is moving from emergency expansion toward more durable, long-term frameworks that will shape future trends in telehealth. That shift directly affects what telehealth services can be offered, how they are reimbursed, and how easily they can scale.
At the same time, some areas remain unsettled. Rules around controlled-substance prescribing, for example, continue to evolve and face increased scrutiny.
For now, the U.S. Department of Health and Human Services (HHS) and the Drug Enforcement Administration (DEA) have extended pandemic-era telemedicine flexibilities for prescribing controlled medications through December 31, 2026. Clinicians can continue prescribing controlled substances via telehealth under certain conditions without a prior in-person visit, while regulators work on a permanent framework.
This does not signal a rollback of telehealth; rather, it suggests that regulatory uncertainty remains part of the operating environment. As a result, many telehealth future trends are less about radical new models and more about building flexibility into how care is delivered and reimbursed.

Why compliance is an ongoing operating requirement
For organizations delivering telehealth, compliance is not a one-time exercise.
Regulation shapes core aspects of the business:
- Which services are reimbursable
- How clinicians can practice across state lines
- What documentation is required
- Which modalities — audio, video, or hybrid — are allowed for specific use cases
Even small policy changes can affect unit economics, staffing models, or care workflows. So, rather than scaling digital health products around a single regulatory interpretation, leading teams design care models and operations that can adapt as rules evolve.
This might mean flexible modality support, configurable workflows, or reimbursement logic that can be updated without redesigning the entire system.
Staying current on regulations is a strategic capability.
Healthcare compliance will continue to shape what can be delivered digitally, how services are paid for, and where sustainable growth is possible. Teams that plan for change — instead of reacting to it — will be better positioned to scale without disruption.
AI moves into infrastructure
Instead of trying to replace clinicians or act like a virtual doctor, AI is settling into a quieter, more practical role: operational infrastructure that makes care easier to deliver.
The biggest gains come from applying AI to everyday tasks that quietly consume clinical time. Intake information is summarized so clinicians don’t start from raw text. Symptoms are routed automatically into the right care pathway. Medical documentation is drafted in the background, cutting down on hours of after-visit charting. Follow-up actions are triggered automatically, so patients receive guidance and monitoring without adding staff workload.
None of this looks dramatic. And that’s the point — 91% of healthcare providers feel positive about using generative AI to ease administrative burden.
Healthcare doesn’t need more impressive demos. In practice, the telehealth future trends that matter most are not the loudest innovations, but the ones that make care more reliable, scalable, and easier to sustain over time.
As investment in health AI matures, attention has shifted away from experimental “AI doctor” concepts and toward tools that reduce workload, improve consistency, and support clinicians rather than compete with them, often with input from AI consulting services.
For teams building telehealth platforms, the priority is straightforward.
AI should be applied where it:
- Saves clinician time
- Standardizes workflows
- Reduces manual effort
- Improves reliability and follow-through
Success should be measured like any other operational improvement: fewer minutes per patient, lower documentation burden, faster routing, and more consistent follow-up.
In 2026, the AI that matters most in telehealth is the kind patients barely notice, and clinicians quietly depend on.
Conclusion
The last five years proved that virtual care can scale. The next phase determines whether it delivers consistent clinical value, sustainable economics, and reliable patient experiences. That shift puts pressure on execution: workflow design, operational discipline, regulatory adaptability, and infrastructure that works quietly in the background.
Organizations that invested early in operational foundations — clear protocols, flexible platforms, and disciplined measurement — will pull ahead quietly. Their advantage will show up in lower costs, better outcomes, and more resilient care delivery.
Building telehealth that works in production is hard — especially when regulation, clinical workflows, and AI all intersect.
At Uptech, we provide healthcare app development services that help companies build telehealth platforms that are secure, compliant, and designed for real clinical use. If you’re planning a new healthcare product or revisiting your telehealth system and want support from a reliable tech partner, let’s talk.